-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
IPSILATERAL FIBULAR TRANSFER: A VALUABLE OPTION FOR TREATMENT OF LARGE TIBIAL DEFECTS IN CHILDREN
Autoři: R. Burda; M. Kitka
Působiště autorů: Department of Trauma Surgery, Faculty Hospital of Louis Pasteur, Košice, Slovak Republic
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 50, 2, 2008, pp. 65-67
CASE REPORT
We present the case of a 6-year-old boy who was struck by a vehicle. He suffered from close femoral fracture AO 32 A1.2 and open tibial fracture AO 42 C3.3 with extensive soft tissue injury on the ipsilateral anterolateral calf (Fig. 1a, 1b, 3, 4).
Obr. 1. a. Tibial shaft fracture – PA view b. Tibial shaft fracture – lateral view c. Tibial defect after debridement and stabilization by unilateral external fixator – PA view d. Tibial defect after debridement and stabilization by unilateral external fixator – lateral view 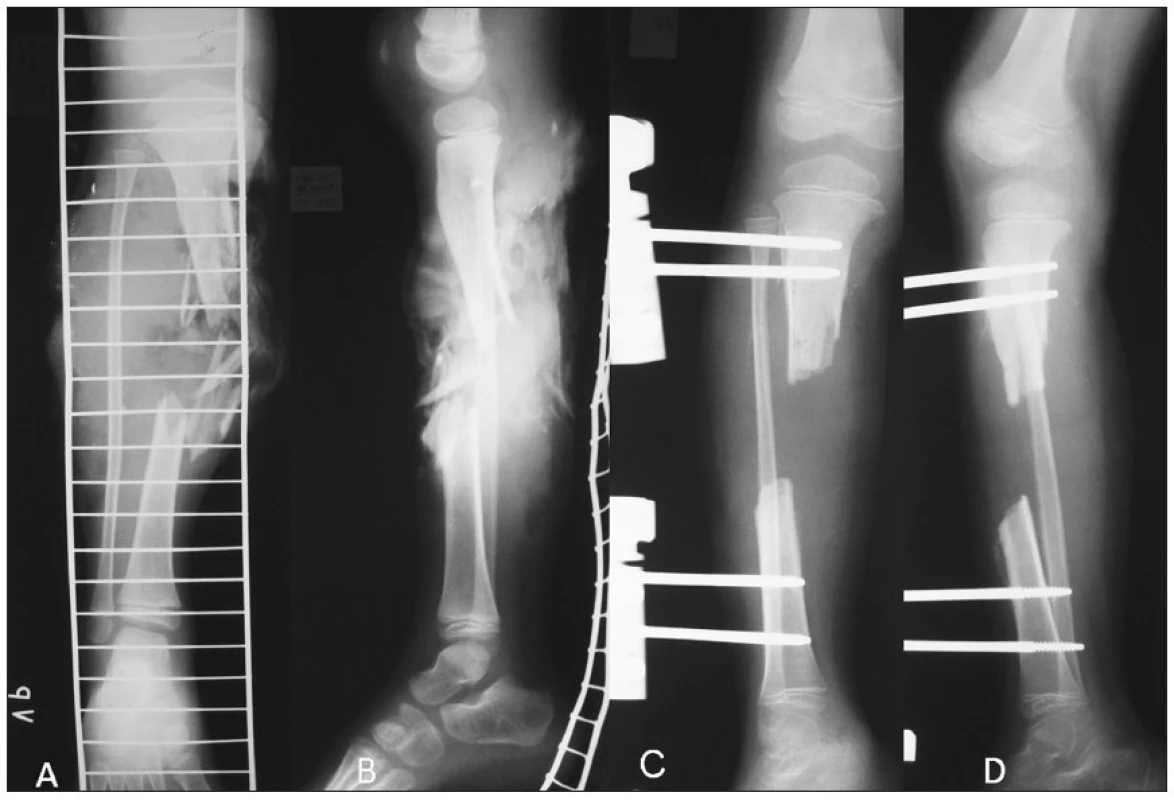
Obr. 2. Soft tissue defects of the calf 
Obr. 3. The extent of bone comminution and soft tissue injury – detail view 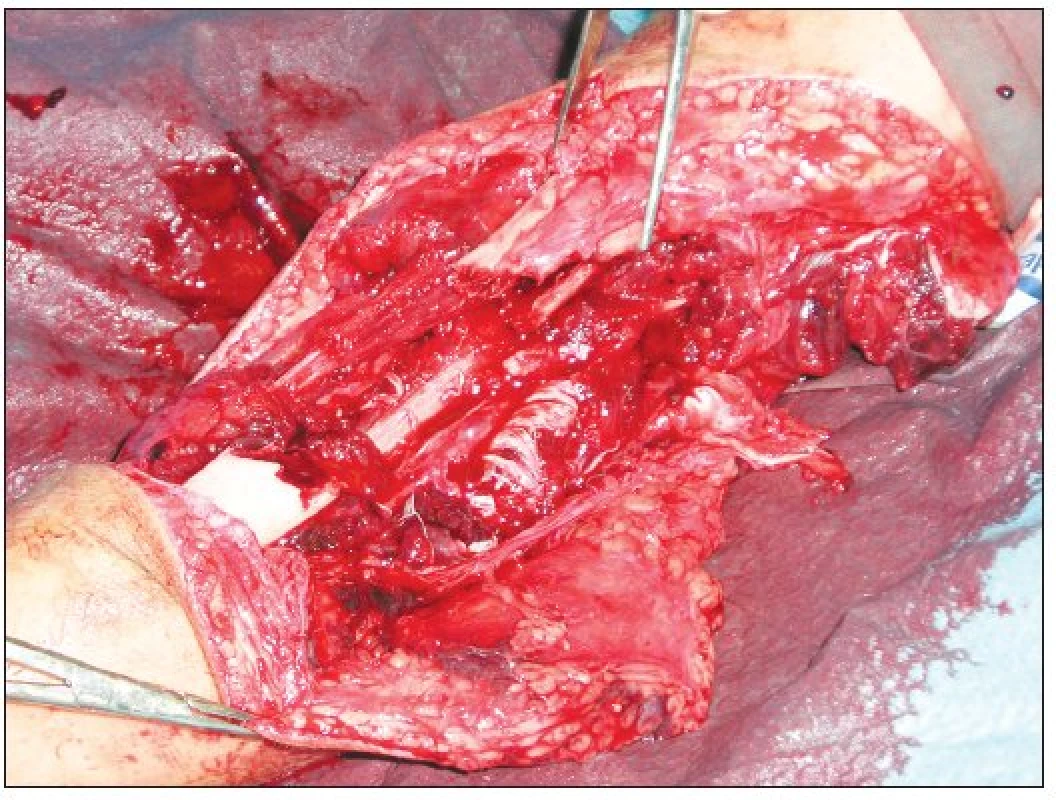
The femoral fracture AO 32 A1.2 was stabilized by open reduction and plate osteosynthesis. Subsequently consistent debridement of the open tibial fracture was carried out. After removal of necrotic tissues and devascularised bone particles, the tibial defect extended to a length of 8 cm (Fig. 1c, 1d). The tibial fracture was stabilized by unilateral external fixator. Remaining skin defects were covered with free skin graft. Early mobilization of knee and ankle joint was begun.
Ipsilateral fibular transfer was chosen as a treatment of choice for this large tibial defect. First stage of transfer was realized 3 weeks after injury. The fibula was approached with a straight lateral approach. The peroneal fascia was incised and the peroneal nerve was visualized and protected before osteotomy. Osteotomy was performed with an oscillating saw 4 cm below the fibular head. The fibula was then gently transposed to the slot in the proximal tibia. The notch in tibia was approximately 2 x 0.5 cm in size. We were not able to make the fibular transposition using one approach. Also anterior approach was needed to fully expose the tibia. The vicinity of the physeal plate forced us to remove the external fixator. The graft was decorticated on the surface adjacent to the tibia, and subsequently screwed to the tibia. An iliac crest cancellous graft was also packed around the proximal anastomosis. External immobilization of the lower limb in a long plaster cast was continued for six weeks. The patient was mobilized on crutches, avoiding weight-bearing. After six weeks the second stage of the procedure was performed. Analogously the distal fibular remnant was transposed to the distal tibia slot. Distal fibular osteotomy was carried out approximately 8 cm above the spike of the lateral malleolus. Fixation was secured with two cortical screws. We wrapped the distal anastomosis with bone chips.
Immobilization of the lower limb continued for another six weeks. Subsequently only short fixation with full weight-bearing was allowed. The fracture completely healed after 5.5 months (Fig. 2a, 2b). X–ray scans revealed progressive hypertrophyof the graftwithout resorption up to twice its original size eight months after fibular transfer. At the 24-month follow up the patient had a tibial lengthening of 2 cm, no varus deformity and a recurvatum deformity of about 20 degrees (Fig. 5, 6). The range of ankle and knee motion is without any restriction.
Obr. 4. a. Two years follow-up – PA view b. Two years follow-up – lateral view 
Obr. 5. Clinical outcome – two years follow-up 
Obr. 6. Clinical outcome – two years follow-up 
DISCUSSION
One of the most difficult problems confronting the reconstructive surgery is the reconstruction of large tibial post-traumatic defects (3). Optimal treatment should permit early mobilisation with weight-bearing, and minimize leg length discrepancy and/or axial deformity (5). These injuries are usually high-energy in nature and are invariably associated with severe soft-tissue damage (4).
Shorter defects measuring up to 5 cm can be treated with either bone transport or corticocancellous bone grafting. For defects longer than 6 cm, most surgeons will use either a free vascularized fibula graft or bone-lengthening techniques (5). The idea of substitution of the tibia with the fibula is based on its function in lower animals, in which the fibula is considered an important support of the leg. In humans due to plantigrade walking it has a less important function. The fibula carries one sixth of the static load of the leg. The fibula undergoes hypertrophy under more than physiological stress and becomes a static supporting element of the leg (1).
The main principle of the ipsilateral fibular transfer lies in fulfilling the gap between the proximal and distal tibial ends by achieving tibiofibular synostosis. The procedure uses a vascularized fibular graft, which evidently speeds up the time of bone healing. The main blood supply to the fibula must remain intact during the procedure. The fibula shaft is supplied by a branch of the peroneal artery, which usually enters the posterior surface of the fibula in the middle third of its shaft, normally 7 cm below its origin, and gives off multiple branches to the periosteum (8).
Ipsilateral vascularized fibula transfer technique has many advantages. It retains periosteal and endosteal vasculature and the main arteries in the leg are left undamaged. No microsurgical skills are required. It offers only minimal donor morbidity and shortens operation time. The technique does not affect growth, so it can be used in children and adolescents. A vascular graft also has greater resistance to infection. Earlier weight-bearing is permitted by the transfer of a large graft of the fibula into a biomechanically advantageous position. It is not very suitable for too proximal or distal tibial defects. This limitation is given by the fact that the main blood supply of the fibula is a branch of the peroneal artery which enters the posterior middle third of the bone 6–7 cm below its origin. The pedicle may be too short for transfer and due to the size of graft, stress fracture may also occur (5).
Main disadvantages include valgus deformity of the donor site ankle (6, 7), development of angular deformity about the knee (2).
Residual stiffness of the ankle after fibular transfer is usually not directly related to the fibular transfer itself. Removal of the fibula does not seem to have any detectable disadvantage in terms of function (4).
There are only a few available references in the literature about the application of ipsilateral fibular transfer in children as a treatment modality for massive traumatic tibial bone loss (2). This option is usually used for treatment of congenital infected non-unions, and as a solution for bone defects after resections of bone tumors in children.
CONCLUSION
Ipsilateral fibular transfer is a relatively old technique which is probably underutilized today. In comparison to other modern techniques, mainly free fibular transfer, it provides comparable results. It seems to be appropriate especially for children and adolescents. We suppose that this method should be still remembered as a valuable option for treatment of large tibial bone defects.
Address for correspondence:
Rastislav Burda, M.D.
Department of Trauma Surgery, Faculty Hospital of Louis Pasteur
Rastislavova 43
040 01 Košice
Slovakia
E-mail: burda@netkosice.sk
Zdroje
1. Agiza AR. Treatment of tibial osteomyelitic defects and infected pseudarthroses by the Huntington fibular transference operation. J. Bone Joint Surg. Am., 63, 1981, p. 814–819.
2. Agus H., Kalenderer O., Eryanilmaz G., Omeroglu H. Biological internal fixation of comminuted femur shaft fractures by bridge plating in children. J. Pediatr. Orthop., 23, 2003, p. 184–189.
3. Hatori M., Ayoub KS., Grimer RJ., Carter SR., Tillman RM. The two stage ipsilateral fibular transfer for tibial defect following tumour excision. Sarcoma, 4, 30, 2000, p. 27–30.
4. Khan MZ., Downing ND., Henry AP. Tibial reconstruction by ipsilateral vascularized fibular transfer. Injury, 27, 1996, p. 651–654.
5. Koulouvaris P., Theos C., Kottakis S., Demertzis N. A simple treatment for a 15-cm tibia bone defect: a case report of an ipsilateral vascularized fibula transfer. J. Orthop. Trauma, 21, 2007, p. 215–218.
6. Ozaki T., Hillmann A., Wuisman P., Winkelmann W. Reconstruction of tibia by ipsilateral vascularized fibula and allograft. 12 cases with malignant bone tumors. Acta Orthop. Scand., 68, 1997, p. 298–301.
7. Pho RW., Levack B., Satku K., Patradul A. Free vascularised fibular graft in the treatment of congenital pseudarthrosis of the tibia. J. Bone Joint Surg. Br., 67, 1985, p. 64–70.
8. Ruch, DS., Koman LA. The fibula-flexor hallucis longus osteomuscular flap. J. Bone Joint Surg. Br., 79, 1997, p. 964–968.
Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2008 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Kombinace paracetamolu s kodeinem snižuje pooperační bolest i potřebu záchranné medikace
- Metamizol v kostce a v praxi – účinné neopioidní analgetikum pro celé věkové spektrum
- Kombinace tramadol/paracetamol zmírňuje bolest v oblasti bederní páteře a může tak zmírnit i depresi
-
Všetky články tohto čísla
- ARTERIALIZED VENOUS FREE FLAPS – A RECONSTRUCTIVE ALTERNATIVE FOR LARGE DORSAL DIGITAL DEFECTS
- RECONSTRUCTION OF LARGE UPPER LIP DEFECTS BY FREE TISSUE TRANSFER
- THE VALUE OF CLINICAL DIAGNOSIS OF DIGITAL GLOMUS TUMORS
- GIANT CELL REPARATIVE GRANULOMA IN THE MANDIBLE – CASE REPORT AND REVIEW OF THE LITERATURE
- IPSILATERAL FIBULAR TRANSFER: A VALUABLE OPTION FOR TREATMENT OF LARGE TIBIAL DEFECTS IN CHILDREN
- ČESKÉ A SLOVENSKÉ SOUHRNY
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- ARTERIALIZED VENOUS FREE FLAPS – A RECONSTRUCTIVE ALTERNATIVE FOR LARGE DORSAL DIGITAL DEFECTS
- GIANT CELL REPARATIVE GRANULOMA IN THE MANDIBLE – CASE REPORT AND REVIEW OF THE LITERATURE
- THE VALUE OF CLINICAL DIAGNOSIS OF DIGITAL GLOMUS TUMORS
- RECONSTRUCTION OF LARGE UPPER LIP DEFECTS BY FREE TISSUE TRANSFER
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



