-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Dietary patterns associated with body mass index (BMI) and lifestyle in Mexican adolescents
Background:
The objetive in this study is to determine the relationship between dietary patterns, BMI, type 2 diabetes mellitus family history (T2DMFH) and some lifestyle variables such as smoking and skipping breakfast in a Mexican adolescent population.Methods:
Cross-sectional, observational, analytical study.Subjetcts: 14-16 years old male and female adolescents (n 373). A previously validated food frequency questionnaire (FFQ) was used and dietary patterns were derived using principal component analysis (PCA). Scores for dietary patterns were categorized by tertiles.Results:
Three major dietary patterns that explained 47 % of variance were found: westernized, high in protein/fat and prudent pattern. Subjects at the highest tertile of prudent pattern had lower BMI. And was also associated with less T2DMFH and less smoking habit when compared with the lowest tertile. We found a positive correlation between BMI and high scores for westernized and high in protein/fat pattern.Conclusions:
Dietary patterns of adolescents are a public health concern because there is a direct association between inadequate diet at this early age and obesity.Keywords:
Dietary patterns, Adolescence, BMI, Lifestyle habits
Authors: Laura Elisa Gutiérrez-Pliego 1,2; Eneida Del Socorro Camarillo-Romero 2; Laura Patricia Montenegro-Morales 2; And José De Jesus Garduño-García 2,3*
Authors place of work: Facultad de Medicina Universidad Autónoma del Estado de México, Av. Paseo Tollocan 48 Universidad, Toluca Estado de México CP501 0, Mexico. 1; Centro de Investigación en Ciencias Médicas UAEMex, Cuerpo académico salud del Universitario Av. Jesús Carranza 205, Universidad, Toluca Estado de México CP 501 0, Mexico. 2; Instituto Mexicano del Seguro Social HGR251, Metepec Estado de, Mexico. 3
Published in the journal: BMC Public Health 2016, 16:850
Category: Research article
doi: https://doi.org/10.1186/s12889-016-3527-6© 2016 The Author(s).
Open access
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
The electronic version of this article is the complete one and can be found online at: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-3527-6Summary
Background:
The objetive in this study is to determine the relationship between dietary patterns, BMI, type 2 diabetes mellitus family history (T2DMFH) and some lifestyle variables such as smoking and skipping breakfast in a Mexican adolescent population.Methods:
Cross-sectional, observational, analytical study.Subjetcts: 14-16 years old male and female adolescents (n 373). A previously validated food frequency questionnaire (FFQ) was used and dietary patterns were derived using principal component analysis (PCA). Scores for dietary patterns were categorized by tertiles.Results:
Three major dietary patterns that explained 47 % of variance were found: westernized, high in protein/fat and prudent pattern. Subjects at the highest tertile of prudent pattern had lower BMI. And was also associated with less T2DMFH and less smoking habit when compared with the lowest tertile. We found a positive correlation between BMI and high scores for westernized and high in protein/fat pattern.Conclusions:
Dietary patterns of adolescents are a public health concern because there is a direct association between inadequate diet at this early age and obesity.Keywords:
Dietary patterns, Adolescence, BMI, Lifestyle habitsBackground
Dietary patterns emerged as an alternative method for the study of the relationship between diet and chronic diseases; traditionally, nutritional epidemiology studies are focused on some diseases and their relation to specifics nutrients or foods [1, 2], moreover people consume food combinations that contain a mixture of nutrients. Dietary patterns analysis focuses on the study of the diet as a whole concept. Its advantage relies in allowing a more complete vision of the diet and its influence on health outcomes, in addition to facilitate comparison between dietary exposures in different cultural groups and population [1,2, 3].
The most common methods used to analyze dietary patterns are: factor analysis (FA), cluster analysis (CA), reduced rank regression (RRR), and principal component analysis (PCA). PCA is the most used trough the world to associate dietary patterns with chronic diseases. Validated food frequency questionnaires (FFQ) and food intake reports are instruments used to derive dietary patterns [2].
Most of the studies regarding dietary patterns have been performed in adult populations. There are few reports in adolescents. It has been suggested that unhealthy dietary patterns are present from early stages of life. The impact on unhealthy outcomes like overweight, obesity or some other metabolic disorder are still controversial in children and adolescents [4, 5, 6]. Despite being widely recognized the importance of establishing healthy eating behaviors early in life, few investigations have been made on dietary patterns in adolescents [7]. This study aims to understand the dietary patterns of adolescents and their relation to different lifestyle variables and body mass index (BMI).
Methods
A cross-sectional, observational, analytic study was conducted in the Medical Sciences Research Center (CICMED, for its acronym in spanish). We invited to participate all first year students, in two high-schools belonging to the Autonomous University of the State of México.
Subjects who accepted to participate were scheduled to an appointment. Parents or guardians were given an informed consent letter to be signed. A physical examination was performed and they were asked to answer a previously validated in Mexican population FFQ [8].
Anthropometric measurement
Weight was obtained with a Tanita® scale, under fasting conditions, with minimal clothing and without shoes, in an upright position, heels together and toes slightly apart. Height was obtained using a Seca® stadiometer placed on the wall forming a 90° angle with the floor, participant was standing in Frankfort plane, without shoes or any object on the head.
The BMI was calculated using data from weight and height (BMI = weight/heigh2) and expressed in kg/m2. The cutoffs used for the study were those proposed by Mercedes de Onis for the World Health Organization (WHO) in 2007 [9] which defines overweight as +1 standard deviation (SD) and obesity as +2SD.
Dietary patterns assessment
A FFQ was given to be answered and the statistical method of principal component analysis (PCA) was used. The questionnaire gathers data of consumption from 116 food items. For each food, a common ration was assigned (e.g. 1 tortilla, 1 apple, etc). Subjects reported the frequency of consumption of such foods in the last six months using ten options of response going from “never” to “6 or more times per day”. Answers were transformed to average daily intake.
For PCA, each questionnaire responses were coded with a value of 0-9 (0 = never, 1 = less than one per month, etc). Food items were categorized into 28 groups based in other studies [10, 11] according to the similarity of nutrients (e.g whole grains, fruits, and desserts) and others were considered individually (e.g tortilla). The answers for each food groups were summed and standardized using Z-score. After that, PCA was carried out using orthogonal transformation (varimax rotation) to reduce the variance, determine dietary patterns and the factor loadings for each food group. Components with an eigenvalue ≥1.5 were retained and factor loadings > .04 were used to describe the component. Finally, dietary patterns were named based on the literature [5, 10, 11, 12, 13]. Subsequently, the factor scores for each participant were used to determine the dietary pattern followed by each subject, and also categorized by tertiles for further analysis.
Other variables
The presence of type 2 diabetes mellitus family history (T2DMFH) was considered if the participant reported that one or more of the parents or grandparents had DM2. Smoking was considered as a minimum consumption of one cigarette per week in the past six months. And skipping breakfast was considered for this study as the lack of breakfast in 4-7 days a week in the past six months.
Statistical analysis
A descriptive analysis of the studied variables was conducted using means and standard deviations for continuous variables. Qualitative variables were expressed as percentage. One-way ANOVA was used to determine differences between BMI and weight across each dietary patterns’ tertile. For qualitative variables such as T2DMFH, smoking and skipping breakfast, a Chi-square test was used. Pearson and Spearman test was conducted as appropriate for analyzing the correlation between BMI and dietary patterns scores. All tests were statistically significant at p < 0.05 and the statistical package used was SPSS 15.0.1.windows Chicago IL USA.
Results
We include 373 participants (160 men, 213 women). The mean age was 14.5 [14, 15, 16] years. The mean BMI was 24.1 ± 3.4 kg/m2, and a mean calorie intake of 8405.4 ± 2937 kJ/day. According BMI 67 % (250 subjects) had normal weight, 24.3 % (91 subjects) had overweight and 8.5 % (32 subjects) had some obesity level. About 11.8 % (44 subjects) reported smoking; 65 % (242 subjects) reported frequent fasting and 37.5 % had at least one close relative (parents or grandparent) with DM2 (Table 1)
Tab. 1. Baseline characteristics 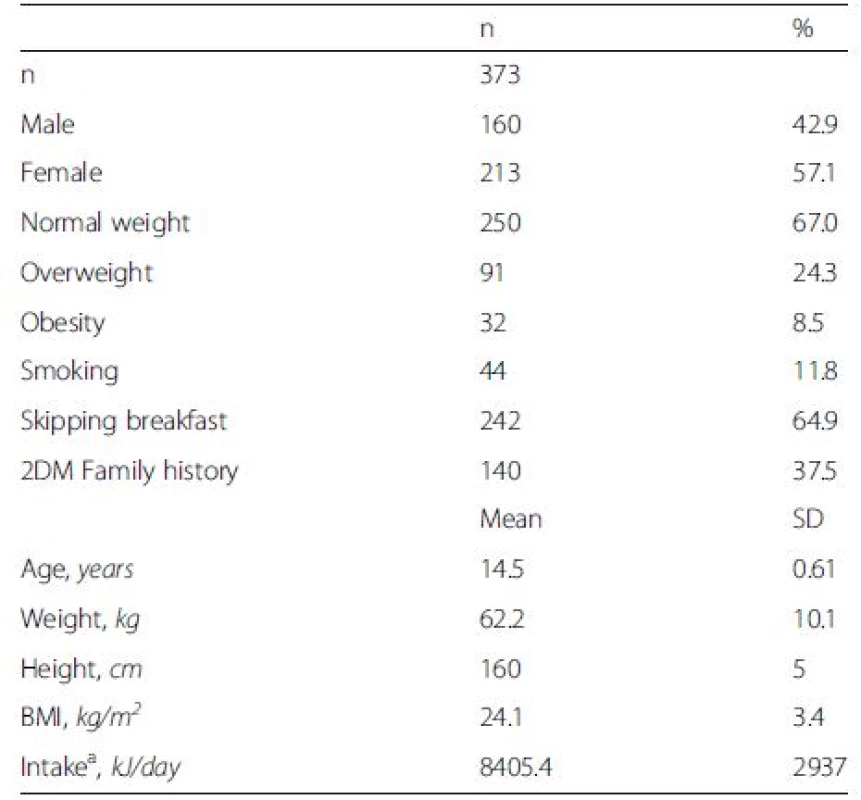
kJ = kilojoules (1 kcal = 4.184 kJ) aDaily intake was calculated according to the FFQ To analyze the validity of the data from each questionnaire, the extreme studentized deviation (ESD) [14] was applied and those questionnaires whose caloric intake was between 2,092 and 27,196 kJ/day were taken as valid.
Prior to PCA, a Kaiser-Meyer-Olkin test of sampling adequacy (.888) and a Bartlett test of sphericity (p < 0.01) was performed to assess whether the factor model as a whole was significant.
Three components or dietary patterns were obtained and named as: 1) Westernized pattern: High intake of refined cereals, snacks, desserts, sweets and sugar, pastries, soda. 2) High in protein/fat pattern (HPF): High consumption of eggs, poultry, red meats, sausages and alcohol. 3) Prudent pattern: High consumption of vegetables, legumes, nuts and seeds, fruits and whole grains. These three major patterns explained 47.3 % of the total variance (Table 2).
Tab. 2. Factor loadings of dietary patterns in Mexican adolescentsa 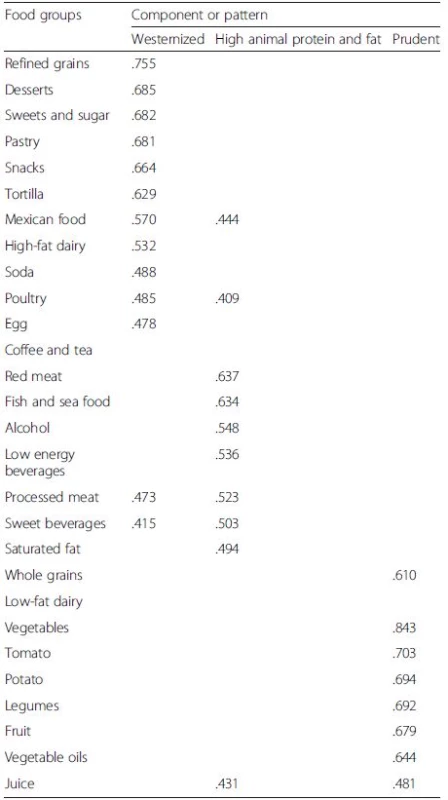
aExtraction method: Principal component analysis (PCA) with varimax rotation Participants in the highest tertiles of Westernized pattern and HPF pattern showed to have a higher BMI compared with those in the highest tertile of the prudent pattern.
As for smoking habit, there was no difference between 1st and 3rd tertiles in unhealthy patterns (westernized and HPF), however, there was less prevalence of smokers in 3rd tertile than 1st tertile of prudent pattern.
It was also found that those participants located in the highest tertile for prudent pattern skipped breakfast more frequently than those at the highest tertiles of unhealthy patterns.
The presence of T2DMFH is associated with unhealthy patterns, it is more common in highest tertiles of unhealthy compared to the highest tertile of prudent pattern (Table 3).Tab. 3. Characteristics of sample across tertiles of dietary patterns 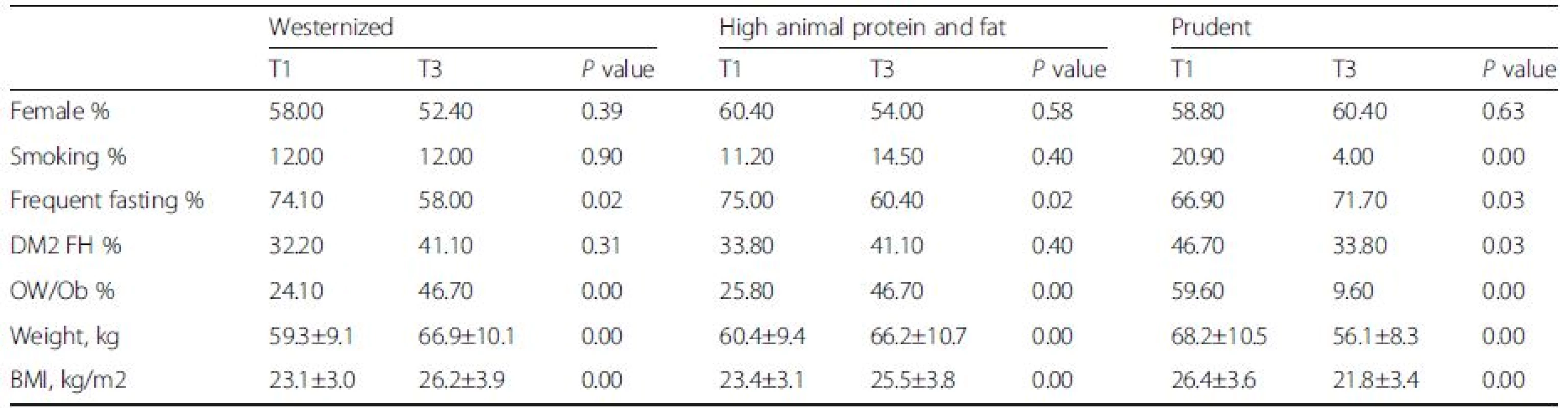
T1: Tertile 1 T3: Tertile 3 OW/Ob: Overweight/Obesity Chi-square test for qualitative data and one way-ANOVA for quantitative data Finally, the Pearson correlation analysis between BMI and the different dietary patterns scores showed a positive correlation with the westernized pattern (r = .316 p < 0.01) and the HPF pattern (r = .307 p < 0.01). In contrast, a negative correlation was found for the prudent dietary pattern (r = -.576 p < 0.01) (Table 4).
Tab. 4. Pearson correlation between BMI and dietary patterns scores 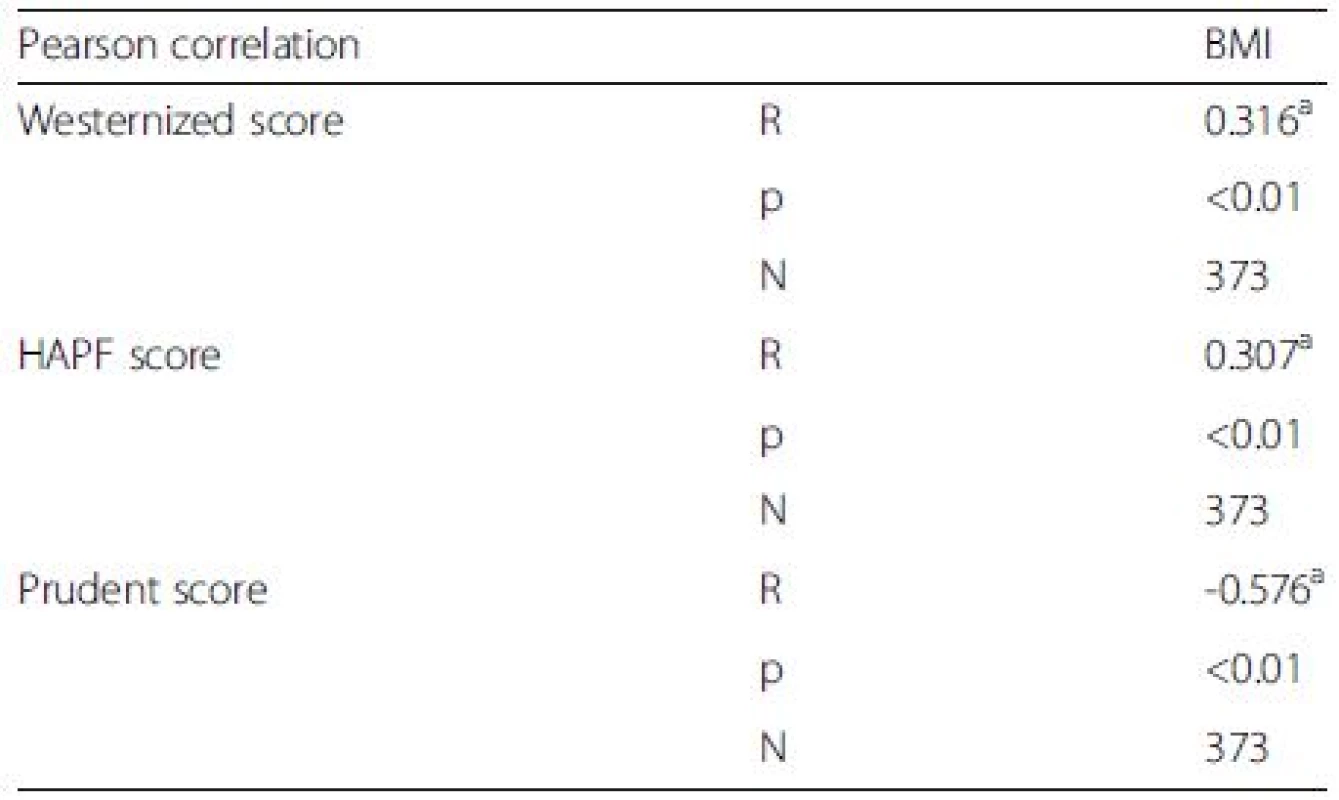
aCorrelation is significative at 0.01 (bilateral) Discussion
In the present study we found that there is a strong relationship between unhealthy dietary patterns (westernized and HPF) and higher BMI in adolescents. In the same way this unhealthy patterns are associated with inadequate eating and lifestyle habits. It was also found that a large number of participants with T2DMFH were following an unhealthy dietary pattern.
Obesity and overweight are considered a global epidemic. As the prevalence of these diseases in children and adolescents is increasing every day in both developed and developing countries [15]. Obesity represents a critical risk factor for many chronic diseases such as type 2 diabetes, cardiovascular disease, hypertension, dyslipidemia, and some type of cancers. Obesity by itself, could be consider a risk factor for mortality. There is an straight correlation between the severity of overweight and mortality risk [16]. From the public health view obesity represents one of the more important or maybe the most important challenge. The International Obesity Task Force estimates the costs of obesity between 2 and 8 % of total health budget [17] In Mexico, the total cost of overweight and obesity (direct and indirect cost) in 2008 was of 67.345 million Mexican pesos and is expected to rise by 2017 to 150.860 million Mexican pesos [18]. Data from the National Survey of Health and Nutrition 2012 (ENSAUT for its acronym in Spanish) reveal that in Mexico, the prevalence of overweight and obesity in adolescents between 12 and 19 years old was 35 %, i.e. 1 in 5 adolescents are overweight, and 1 in 10 are obese [19]. When analyzing the prevalence of overweight and obesity in this study, a similar data was found (32.9 %), which places this population slightly below the national mean. It is extremely relevant to describe all phenomena related to obesity in Mexican adolescents. It has been described that Mexican children and adolescents has the higher increasing trend in the prevalence of obesity and overweight all over the world [20]. The most serious consequences of obesity in adolescents will appear until adulthood (out of 3 obese children, one adult will remain so) because of severe comorbidities [21].
Overweight and obesity results from the interaction of different genetic, environmental and lifestyle factors [22] Considering the genetic factor, it is known that if both parents are obese, the risk of obesity in children will be from 69-80 % when only one parent is obese the risk will be of 41-50 % and conversely if neither parent is obese, the risk decreases to 9 % [23]. However it is considered that the most important factor in the development of such diseases corresponds to lifestyle, specially diet and physical activity have important influence on the development of overweight and obesity [24].
One aspect closely linked to obesity is undoubtedly food. Human consumption is an act in which diverse phenomena of nature are combined, as it includes a set of social and biological interactions mediated by the culture in which it takes place [25]. Eating habits in adolescence has a biological and cultural nature, the first one is related to growth and biological development and the second with formation of beliefs and daily practices according to social influences such as friends, school, media and family. Both aspects determine current and future stages of teenage life [26]. During adolescence, many physical and psychological changes occur that modifies dietary patterns and physical activity habits, which means that if a good match between the needs (as a consequence of age, development and new lifestyle) and the energy intake does not occur, teens will have a great likelihood of eating disorders either by default (anorexia, bulimia) or excess (overweight and obesity) [27]. In the present study we can identify certain meal habits that are present since this early stages of life. And we also describe how this habits are associated with weight.
The analysis of dietary patterns emerged as an alternative to the study of the diet and its relation to various health outcomes; however, these studies have been done mostly in adults and mayors, finding consistency in dietary patterns derived. Regarding dietary patterns found in previous studies performed in adult populations in the world. It has been identified three consistent dietary patterns: the prudent or healthy dietary pattern characterized by a high consumption of fruits , vegetables, whole grains and fish [28, 29, 30,31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42]; the westernized or unhealthy patter characterized by low consumption of fruits, vegetables and high consumption of refined grains, processed food, pastry and high-fat diary [33, 34, 35, 37, 38, 39, 40, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52]; and a third dietary patter called High in protein/fat pattern defined by a high intake of dairy, eggs, red meat, processed meat, poultry and low consumption of fruits, vegetables and whole grains [29, 32, 36, 41, 42, 45, 53, 54, 55, 56, 57, 58]. This study is one of the first made in adolescent population, and has identified three major dietary patterns similar to those found in other studies in adults. The similarity found between dietary patterns of adolescents and adults suggests that behaviors early in life remain largely unchanged until adulthood.
By analyzing the relationship between BMI and dietary patterns, it was found that the higher the score of unhealthy patterns, the higher the BMI, and conversely, the higher the score in prudent pattern, the lower was the BMI. This results suggest that although weight gain is determined by food consumption from a quantitative view, it is also the qualitative aspect which needs more attention.
The present study provides evidence that adolescents with higher scores of unhealthy dietary patterns are not only associated with weight, another cardiovascular risk factors like smoke are seen in patients with higher scores of unhealthy patterns. These results are consistent with a study that described that teens who smoked tended to eat fewer vegetables, dairy and exercise less [59]. The results of this study show that a high percentage of the population has the habit of skipping breakfast (regardless of dietary pattern to follow). The literature states that skipping breakfast is a risk factor for being overweight or obese and it is possible that the information that adolescents have about the consequences of skipping breakfast is incomplete or wrong [60, 61].
It is known that the family has a strong influence on the diet of children and adolescents and also on their food-related behaviors. This influence can have a significant impact on weight gain. The association of the presence of T2DMFH and unhealthy patterns can be explained considering that each cultural group transmits their eating habits from generation to generation through food education to their children, regardless of whether is healthy or not [62].
The strength of this study is that is one of the first studies designed to analyze dietary patterns in adolescents and it is performed in one of the most high prevalence of obesity population in the world. The weakness of this study is the cross sectional design.
Conclusions
Dietary patterns of adolescents are a public health concern because there is a direct association between inadequate diet at this early age and obesity. Therefore, adolescence is a good stage to intervene in changing dietary patterns and the consolidation of a healthy lifestyle that the teenager will keep until adulthood and which in turn will transmit to future generations. With advances in the study of dietary patterns, the development of effective strategies focused on changing patterns that could provide a clear starting point in the prevention and treatment of various diseases such as overweight and obesity in adolescents should emerge.
Acknowledgements
The authors are grateful to the study subjects who participated in this project and to the Medical Sciences Research Center staff for the facilities provided.
Funding
Source of funding: The present study was supported by PROMEP 2013: Fortalecimiento de cuerpos académicos for the project "Identification of early metabolic abnormalities in adolescents with risk factors." Registration No. CA-186, agreement 103105/13/9057.
Availability of data and materials
According to public research policies regarding to research the could not be public available.
Authors’ contributions
LEGP executed the research procedures, sample collection, laboratory analyses, and data interpretation, designed the study, clinical management, and laboratory analyses; interpreted data; contributed to the discussion; and reviewed and edited the manuscript. JJGG designed the study, interpreted data, contributed to the discussion; and reviewed and edited the manuscript. LPMM designed the study, executed the research procedures, sample collection, contributed to the discussion and reviewed and edited the manuscript. ESCM designed the study, executed the research procedures, sample collection, laboratory analyses, and interpreted data, contributed to the discussion and reviewed and edited the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients. The protocol were approved by the Research and Ethics committee from the Medical Science Research Center UAEM. ID number (2015/04). Written informed consent was obtained from all subjects/patients.
Abbreviations
BMI, Body Mass Index; CA, Cluster Analysis; FA, Factor Analysis; FFQ, Food Frequency Questionaries’; HPF, High in Protein/Fat Pattern; PCA, Principal Components Analysis; RRR, Reduced Rank Regression; SD, Standar Deviations; T2DMFH, Type 2 diabetes Family History
Received: 14 January 2016
Accepted: 20 June 2016
Published: 22 August 2016* Correspondence:
José de Jesus Garduño-García
2Centro de Investigación en Ciencias Médicas UAEMex,
Cuerpo académico salud del Universitario Av. Jesús Carranza 205, Universidad,
Toluca Estado de México CP 50130, Mexico3Instituto Mexicano del Seguro Social HGR251,
Metepec Estado de, Mexicojjgg1977@hotmail.com
Zdroje
1. Aldana MF. Aplicaciones, dificultades y perspectivas del uso de patrones dietarios para entender la relación entre dieta y salud. Salud Publica Mex. 2007;49 : 106.
2. Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13 : 3–9.
3. Kant AK. Dietary patterns and health outcomes. J Am Diet Assoc. 2004;104 : 615–35.
4. Pinho L, Silveira MF, Botelho ACC, et al. Identification of dietary patterns of adolescents attending public schools. J Pediatr (Rio J). 2014;90 : 267–72.
5. Romero-Polvo A, Denova-Gutierrez E, Rivera-Paredez B, et al. Association between dietary patterns and insulin resistance in Mexican children and adolescents. Ann Nutr Metab. 2012;61 : 142–50.
6. Lozada AL, Flores M, Rodríguez S, et al. Patrones dietarios en adolescentes mexicanas. Una comparación de dos métodos. Encuesta Nacional de Nutrición, 1999. Salud Publica Mex. 2007;49 : 263–73.
7. Matthys C, De Henauw S, Devos C, et al. Estimated energy intake, macronutrient intake and meal pattern of Flemish adolescents. Eur J Clin Nutr. 2003;57 : 366–75.
8. HernÁNdez-Avila M, Romieu I, Parra S, et al. Validity and reproducibility of a food frequency questionnaire to assess dietary intake of women living in Mexico City. Salud Publica Mex. 1998;40 : 133–40.
9. de Onis M, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85 : 660–7.
10. Denova-Gutierrez E, Castanon S, Talavera JO, et al. Dietary patterns are associated with metabolic syndrome in an urban Mexican population. J Nutr. 2010;140 : 1855–63.
11. Denova-Gutierrez E, Castanon S, Talavera JO, et al. Dietary patterns are associated with different indexes of adiposity and obesity in an urban Mexican population. J Nutr. 2011;141 : 921–7.
12. Denova-Gutiérrez E, Castañón S, Talavera JO, et al. Dietary Patterns Are Associated with Metabolic Syndrome in an Urban Mexican Population. J Nutr. 2010;140(10):1855-63.
13. Denova-Gutierrez E, Hernandez-Ramirez RU, Lopez-Carrillo L. Dietary patterns and gastric cancer risk in Mexico. Nutr Cancer. 2014;66 : 369–76.
14. Rosner B. Percentage points for a generalized ESD many-outlier procedure. Technometrics. 1983;25 : 165–72.
15. Proimos J, Sawyer S. Obesity in childhood and adolescence. Aust Fam Physician. 2000;29 : 321–7.
16. Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and mortality in a prospective cohort of US adults. New England J Med. 1999;341 : 1097–105.
17. Rossner S. Obesity: the disease of the twenty-first century. Int J Obes Relat Metab Disord. 2002;26 Suppl 4:S2–4.
18. Rtveladze K, Marsh T, Barquera S, et al. Obesity prevalence in Mexico: impact on health and economic burden. Public Health Nutr. 2014;17 : 233–9.
19. Gutierrez JP, Rivera-Dommarco J, Shamah-Levy T, et al. Encuesta nacional de salud y nutrición 2012. Resultados Nacionales Cuernavaca: Instituto Nacional de Salud Pública; 2012.
20. Lobstein T, Jackson-Leach R, Moodie ML, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385(9986):2510-20.
21. Marcos Sánchez A. Alimentación y valoración del estado nutricional de los adolescentes españoles (Estudio AVENA). Evaluación de riesgos y propuesta de intervención. I. Descripción metodológica del proyecto. Nutr Hosp. 2003;18 : 15–28.
22. Gomez Perez FJ, Rios JM, Aguilar-Salinas C. Posición de la Sociedad Mexicana de Nutrición y Endocrinología sobre el manejo del síndrome metabólico. Revista de Endocrinología y Nutrición. 2005;13 : 9–23.
23. Katzmarzyk PT, Pérusse L, Rao DC, et al. Familial risk of overweight and obesity in the Canadian population using the WHO/NIH criteria. Obes Res. 2000;8 : 194–7.
24. Martínez-Munguía C, Navarro-Contreras G. [Psychological, social and cultural factors of overweight and obesity in children and adolescents in México]. Rev Med Inst Mex Seguro Soc. 2014;52 Suppl 1:S94-101.
25. Aguilar P. Una visión integral de la alimentación: cuerpo, mente y sociedad. Cuadernos de Nutrición. 2002;25.
26. Murillo OO, Consuelo M, Rey PA. Panorama de prácticas de alimentación de adolescentes escolarizados Overview of feeding practices in school adolescents Panorama de práticas de alimentação. Avances en enfermería. 2009;27.
27. Marcos A, Montero A, López-Varela S, et al. Eating disorders (obesity, anorexia nervosa, bulimia nervosa), immunity, and infection. Nutr Immun Infect Infants Child. 2001;45 : 243–62.
28. Markaki I, Linos D, Linos A. The influence of dietary patterns on the development of thyroid cancer. Eur J Cancer. 2003;39 : 1912–9.
29. Newby PK, Muller D, Hallfrisch J, et al. Dietary patterns and changes in body mass index and waist circumference in adults. Am J Clin Nutr. 2003;77 : 1417–25.
30. Shimizu K, Takeda S, Noji H, et al. Dietary patterns and further survival in Japanese centenarians. J Nutr Sci Vitaminol. 2003;49 : 133–8.
31. Appel LJ, Miller ER, Jee SH, et al. Effect of dietary patterns on serum homocysteine results of a randomized, controlled feeding study. Circulation. 2000;102 : 852–7.
32. McCann SE, Marshall JR, Brasure JR, et al. Analysis of patterns of food intake in nutritional epidemiology: food classification in principal components analysis and the subsequent impact on estimates for endometrial cancer. Public Health Nutr. 2001;4 : 989–97.
33. Osler M, Heitmann BL, Gerdes LU, et al. Dietary patterns and mortality in Danish men and women: a prospective observational study. Br J Nutr. 2001;85 : 219–25.
34. Terry P, Hu FB, Hansen H, et al. Prospective study of major dietary patterns and colorectal cancer risk in women. Am J Epidemiol. 2001;154 : 1143–9.
35. Terry P, Suzuki R, Hu FB, et al. A prospective study of major dietary patterns and the risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2001;10 : 1281–5.
36. Williams DEM, Prevost AT, Whichelow MJ, et al. A cross-sectional study of dietary patterns with glucose intolerance and other features of the metabolic syndrome. Br J Nutr. 2000;83 : 257–66.
37. Hu FB, Rimm E, Smith-Warner SA, et al. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr. 1999;69 : 243–9.
38. Hu FB, Rimm EB, Stampfer MJ, et al. Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr. 2000;72 : 912–21.
39. Fung TT, Rimm EB, Spiegelman D, et al. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am J Clin Nutr. 2001;73 : 61–7.
40. Slattery ML, Boucher KM, Caan BJ, et al. Eating patterns and risk of colon cancer. Am J Epidemiol. 1998;148 : 4–16.
41. Chen H, Ward MH, Graubard BI, et al. Dietary patterns and adenocarcinoma of the esophagus and distal stomach. Am J Clin Nutr. 2002;75 : 137–44.
42. Huijbregts PP, Feskens EJM, Kromhout D. Dietary patterns and cardiovascular risk factors in elderly men: the Zutphen Elderly Study. Int J Epidemiol. 1995;24 : 313–20.
43. Newby PK, Weismayer C, Åkesson A, et al. Long-term stability of food patterns identified by use of factor analysis among Swedish women. J Nutr. 2006;136 : 626–33.
44. Kerver JM, Yang EJ, Bianchi L, et al. Dietary patterns associated with risk factors for cardiovascular disease in healthy US adults. Am J Clin Nutr. 2003;78 : 1103–10.
45. Masaki M, Sugimori H, K-i N, et al. Dietary patterns and stomach cancer among middle-aged male workers in Tokyo. Asian Pac J Cancer Prev. 2003;4 : 61–6.
46. Sánchez-Villegas A, Delgado-Rodriguez M, Martínez-González MÁ, et al. Gender, age, socio-demographic and lifestyle factors associated with major dietary patterns in the Spanish Project SUN (Seguimiento Universidad de Navarra). Eur J Clin Nutr. 2003;57 : 285–92.
47. Sichieri R. Dietary patterns and their associations with obesity in the Brazilian city of Rio de Janeiro. Obes Res. 2002;10 : 42–8.
48. Fung TT, Willett WC, Stampfer MJ, et al. Dietary patterns and the risk of coronary heart disease in women. Arch Intern Med. 2001;161 : 1857–62.
49. Osler M, Helms Andreasen A, Heitmann B, et al. Food intake patterns and risk of coronary heart disease: a prospective cohort study examining the use of traditional scoring techniques. Eur J Clin Nutr. 2002;56 : 568–74.
50. Diehr P, Beresford SAA. The relation of dietary patterns to future survival, health, and cardiovascular events in older adults. J Clin Epidemiol. 2003;56 : 1224–35.
51. Martikainen P, Brunner E, Marmot M. Socioeconomic differences in dietary patterns among middle-aged men and women. Soc Sci Med. 2003;56 : 1397–410.
52. Tsai Y-Y, McGlynn KA, Hu Y, et al. Genetic susceptibility and dietary patterns in lung cancer. Lung Cancer. 2003;41 : 269–81.
53. Millen BA, Quatromoni PA, Copenhafer DL, et al. Validation of a dietary pattern approach for evaluating nutritional risk: the Framingham Nutrition Studies. J Am Diet Assoc. 2001;101 : 187–94.
54. Newby PK, Muller D, Tucker KL. Associations of empirically derived eating patterns with plasma lipid biomarkers: a comparison of factor and cluster analysis methods. Am J Clin Nutr. 2004;80 : 759–67.
55. Tseng M, Breslow RA, DeVellis RF, et al. Dietary patterns and prostate cancer risk in the National Health and Nutrition Examination Survey Epidemiological Follow-up Study cohort. Cancer Epidemiol Biomarkers Prev. 2004;13 : 71–7.
56. Whichelow MJ, Prevost AT. Dietary patterns and their associations with demographic, lifestyle and health variables in a random sample of British adults. Br J Nutr. 1996;76 : 17–30.
57. Handa K, Kreiger N. Diet patterns and the risk of renal cell carcinoma. Public Health Nutr. 2002;5 : 757–67.
58. Maskarinec G, Novotny R, Tasaki K. Dietary patterns are associated with body mass index in multiethnic women. J Nutr. 2000;130 : 3068–72.
59. Wilson DB, Smith BN, Speizer IS, et al. Differences in food intake and exercise by smoking status in adolescents. Prev Med. 2005;40 : 872–9.
60. Sjöberg A, Hallberg L, Höglund D, et al. Meal pattern, food choice, nutrient intake and lifestyle factors in The Göteborg Adolescence Study. Eur J Clin Nutr. 2003;57 : 1569–78.
61. Croezen S, Visscher TLS, Ter Bogt NCW, et al. Skipping breakfast, alcohol consumption and physical inactivity as risk factors for overweight and obesity in adolescents: results of the E-MOVO project. Eur J Clin Nutr. 2009;63 : 405–12.
62. Busdiecker B, Castillo D, Salas A. Cambios en los hábitos de alimentación durante la infancia: una visión antropológica. Rev Chil Pediatr. 2000;71 : 5–11.
Článok vyšiel v časopiseBMC Public Health
Najčítanejšie tento týždeň
2016 Číslo 850- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejasný stín na plicích – kazuistika
- Masturbační chování žen v ČR − dotazníková studie
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Eliquis (apixaban) nově hrazen ze zdravotního pojištění
Najčítanejšie v tomto čísle
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



