-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Mini-invasive technique of sclerotherapy with talc in chronic seroma after abdominoplasty – a case report and literature review
Authors: R. M. Palacios Huatuco; Ramírez F. M.; Sala F. H.; Mayer F. H.
Authors place of work: Plastic Surgery Department, Hospital Italiano de Buenos Aires, University of Buenos Aires School of Medicine, Hospital Italiano de Buenos Aires University Institute, Buenos Aires, Argentina
Published in the journal: ACTA CHIRURGIAE PLASTICAE, 64, 3-4, 2022, pp. 143-147
doi: https://doi.org/10.48095/ccachp2022143Introduction
Abdominoplasty is one of the most common cosmetic surgeries performed worldwide [1]. As with any other surgical intervention, both abdominoplasties and lipoabdominoplasties are susceptible to complications [2]. Seroma formation is one of the most frequent complications and has been reported in about 5–30% of cases [3]. Although seromas are usually resolved with multiple aspirations, they can sometimes become chronic, leading to the development of a pseudocapsule or pseudobursa [4]. Talc seromadesis is inspired by pleurodesis and is a widely accepted technique to treat pleural effusion and recurrent pneumothorax [5]. Therefore, it seems to be an easily reproducible and attractive technique that would allow the definitive treatment of recurrent seromas. We present the first report of chronic seroma after lipoabdominoplasty that was successfully treated with talc sclerosis.
Description of the case
A 59-year-old man with a history of grade 1 obesity (Body Mass Index (BMI) 32.4 kg/m2), high blood pressure, atrial fibrillation, and a former smoker. Liposuction and abdominoplasty were performed due to lipodystrophy, abdominal flaccidity, and recti diastasis. The surgery did not present immediate complications and the wound was closed with two suction drains that were removed 7 and 10 postoperative days when the volumes were < 30 mL in 24 hours. However, on postoperative day 30, the patient developed a large subcutaneous seroma (Fig. 1), which was aspirated, obtaining 360 mL. Subsequently, the treatment of the seroma required compression methods and 10 ultrasound-guided punctures, with a medium aspirated volume of 213 mL (range 48–400) for 7 months. Due to the persistent behavior of the seroma, the patient underwent surgery. As an intraoperative finding, a bursa was identified that was debrided with its entire pseudocapsule. The liquid samples were sent for microbiological culture that did not show development and for histopathological study that reported a whitish tissue of 16 × 12.5 cm corresponding to fibroconnective tissue. Twenty-eight days after the surgery, the patient continued with induration and fluctuation at the incision site. Therefore, we decided to perform percutaneous sclerosis with talc.
Fig. 1. Ultrasound with liquid collection in the subcutaneous plane of 15 × 13 cm in the transverse direction and craniocaudal of 1.4 cm thick (red arrow). 
Surgical technique
Ultrasound technology produces noninvasive high-resolution imaging and is considered a valuable tool to identify and assess fluid collections [6]. Under ultrasound guidance and local anesthesia, the seroma was punctured and an 8.5 Fr multipurpose drainage catheter (Fig. 2) was placed using the Seldinger technique. Once the content was evacuated, a suspension of 5 g of talc was instilled in 50 mL of saline solution through the catheter (Fig. 3). The catheter remained closed for 6 hours to promote sclerosis and adhesion of the cavity walls. It was associated with a compressive bandage. Both the procedure and the patient's recovery were without complications. Fourteen days after the procedure, the catheter was withdrawn with a volume of < 10 mL in 24 hours and no adverse effects were reported.
Fig. 2. An 8.5-Fr multipurpose drainage catheter set (Cook Medical Inc., Bloomington, IN). 
Fig. 3. Ultrasound-guided puncture and drainage of the collection with a catheter (red arrow) with subsequent instillation of talc. 
The monitoring was followed up for up to 2 years after sclerotherapy. Control computed tomography showed fibrotic changes in the subcutaneous plane of the abdominal wall (Fig. 4). The patient is currently progressing well without recurrence of the seroma.
Fig. 4. Control 2 years after sclerotherapy. Computed tomography of the abdomen and pelvis shows fibrosis in the subcutaneous plane with resolution of the seroma (red arrow). 
Discussion
Abdominoplasty, also known as a tummy tuck, is a surgical procedure that consists of removing excess fat and skin around the abdomen and strengthening the muscles of the abdominal wall [7]. According to the American Society of Plastic Surgeons (ASPS) report, abdominoplasty was considered the fourth most performed aesthetic surgical procedure in 2020 [8]. Although men are increasingly undergoing this type of surgery, it remains more prevalent in women [8]. This coincides with our institutional experience.
Despite the popularity of abdominoplasty, it carries a higher risk of complications compared to other cosmetic procedures. These complications include hemorrhage, surgical site infection, wound dehiscence, skin or fat necrosis, hematoma, pulmonary embolism, and seroma [9]. BMI, and association with liposuction are the most important predictive factors to seroma formation after abdominoplasty [10]. Both factors were present in our patient.
Seromas are indeed common complications faced by plastic surgeons [11]. In a systematic review and meta-analysis, the global prevalence of seroma after abdominoplasty was reported to be 10.9% [10]. If a seroma is not detected or treated properly, it can develop a fibrous pseudocapsule that transforms the seroma into a chronic encapsulated condition [12]. Our patient developed a seroma refractory to multiple aspirations for a prolonged period. When a seroma persists despite successive drainages, it becomes a difficult problem to solve and causes a significant deterioration in the quality of life of the patient, and increases the costs of hospital care [10,13].
In order to reduce post-operative seroma formation several measures have been proposed, including prolonged use of drainages, compressive garments, tissue glue and progressive tension sutures [14]. In the same fashion, in 1998 Baroudi and Ferreira described the quilting suture technique where sutures bite the muscular fascia below and the superficial fascia of the skin flap above to effectively reduce shearing forces, dead space and consequentely the incidence of seroma [15].
Currently, there is no consensus on the treatment of symptomatic seroma, it varies from percutaneous aspiration to surgical drainage or instillation of sclerosing substances [13]. In this case, the excision of the seroma cavity and pseudocapsule was also performed. However, treatment was insufficient, probably due to its size, chronic behavior, and the omission of progressive tension or quilting sutures after pseudocapsula resection. Therefore, we decided to perform percutaneous talc sclerosis.
Sclerotherapy is a procedure that uses a chemical agent to irritate the inner lining of a seroma, inducing an inflammatory reaction that leads to fibrosis and collapse of the cavity [11]. Recommendations are derived from literature on thoracic surgery addressing pleural effusions [16].
So far, eight studies on talc sclerotherapy for chronic seromas have been reported [5,13,17–22] in various surgical specialties (Tab. 1). We found that 57% were men with a mean age of 40.8 years. A total of 47.6% were chronic seromas after abdominal wall surgeries. The need for aspirations was described in 85.7%. In one case, initial treatment was insufficient and surgical decortication was added. The most used presentation of talc was 4 g of dry powder. Complications were described in 9.5% and sclerotherapy failure was reported in 7 patients. Our case presented some characteristics similar to those reports in the literature. However, we did not find published reports on the usefulness of talc sclerosis in the treatment of chronic seromas related to abdominoplasty.
Tab. 1. List of published cases of talc-induced sclerosis in the treatment of chronic seromas. 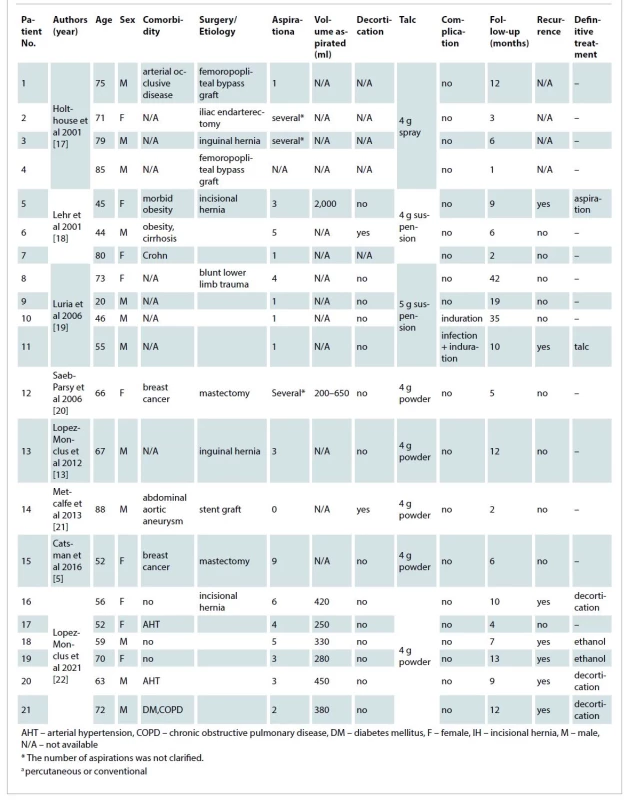
Conclusions
Talc percutaneous sclerosis could be considered as a safe and minimally invasive technique for the treatment of chronic seroma after abdominoplasty when other surgical alternatives fail to solve the problem. To the best of our knowledge, this is the first successful case reported in medical literature. However, more evidence is required to standardize its applicability.
Roles of authors
René M. Palacios Huatuco and Mariano F. Ramírez (literature review, writing the paper, and interpretation);
Hernán F. Sala (literature review, and data analysis);
Horacio F. Mayer (literature review, study concept, and approved the final version).
Conflict of interest: The authors declare that they have no conflict of interest.
Disclosure: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The local Research Ethics Committee has confirmed that no ethical approval is required for case reports.
Patient consent: Patient signed informed consent regarding publishing her data and images.
Horacio F. Mayer, MD, FACS
Hospital Italiano de Buenos Aires
Perón 4190, 1st. floor (1181)
Buenos Aires
Argentina
e-mail: horacio.mayer@hospitalitaliano.org.ar
Submitted: 22. 6. 2022
Accepted: 11.1.2023
Zdroje
1. The International Society of Aesthetic Plastic Surgery. ISAPS International Survey on Aesthetic/Cosmetic Procedures Performed in 2014. Int Soc Aesthetic Plast Surg. 2015, 1–18.
2. Vidal P., Berner JE., Will PA. Managing complications in abdominoplasty: a literature review. Arch Plast Surg. 2017, 44(5): 457–468.
3. Stewart KJ., Stewart DA., Coghlan B., et al. Complications of 278 consecutive abdominoplasties. J Plast Reconstr Aesthetic Surg. 2006, 59(11): 1152–1155.
4. Caulfield RH., Maleki-Tabrizi A., Khan F., et al. A large encapsulated seroma presenting as a mass 5 years post paraumbilical hernia repair. J Plast Reconstr Aesthetic Surg. 2009, 62(1): 105–107.
5. Catsman CJLM., Beek MA., Rijken AM. Talc seromadesis in patients with chronic seroma formation after breast surgery. Springerplus. 2016, 5 : 3.
6. Mortada H., Al Mazrou F., Alghareeb A., et al. Overview of the role of ultrasound imaging applications in plastic and reconstructive surgery: is ultrasound imaging the stethoscope of a plastic surgeon? A narrative review of the literature. Eur J Plast Surg. 2022.
7. Rosenfield LK., Davis CR. Evidence-based abdominoplasty review with body contouring algorithm. Aesthetic Surg J. 2019, 39(6): 643–661.
8. American Society of Plastics Surgeons. 2014 Plastic Surgery Statistics Report. Am Soc Plast Surg. 2014, 1–23.
9. Murshid M., Khalid KN., Shakir A., et al. Abdominoplasty in obese and in morbidly obese patients. J Plast Reconstr Aesthetic Surg. 2010, 63(5): 820–825.
10. Salari N., Fatahi B., Bartina Y., et al. The global prevalence of seroma after abdominoplasty: a systematic review and meta-analysis. Aesthetic Plast Surg. 2021, 45(6): 2821–2836.
11. Sood A., Kotamarti VS., Therattil PJ., et al. Sclerotherapy for the management of seromas: a systematic review. Eplasty. 2017, 17: e25.
12. Roje Z., Roje Ž., Karanović N., et al. Abdominoplasty complications: a comprehensive approach for the treatment of chronic seroma with pseudobursa. Aesthetic Plast Surg. 2006, 30(5): 611–615.
13. Lopez-Monclus J., Garcia-Urẽa MA., Blázquez LA., et al. Persistent inguinal seroma managed with sprinkling of talcum powder: a case report. J Med Case Rep. 2012, 6 : 391.
14. Jabbour S., Awaida C., Mhawej R., et al. Does the addition of progressive tension sutures to drains reduce seroma incidence after abdominoplasty? A systematic review and meta-analysis. Aesthetic Surg J. 2017, 37(4): 440–447.
15. Baroudi R., Ferreira CAA. Seroma: how to avoid it and how to treat it. Aesthetic Surg J. 1998, 18(6): 439–441.
16. Janis JE., Khansa L., Khansa I. Strategies for postoperative seroma prevention: a systematic review. Plast Reconstr Surg. 2016, 138(1): 240–252.
17. Holthouse DJ., Chleboun JO. Talc serodesis – report of four cases. J R Coll Surg Edinb. 2001, 46(4): 244–245.
18. Lehr SC., Schuricht AL. A minimally invasive approach for treating postoperative seromas after incisional hernia repair. JSLS. 2001, 5(3): 267–271.
19. Luria S., Yaakov A., Yoram W., et al. Talc sclerodhesis of persistent Morel-Lavallée lesions (posttraumatic pseudocysts): case report of 4 patients. J Orthop Trauma. 2006, 20(6): 435–438.
20. Saeb-Parsy K., Athanassoglou V., Benson JR. Talc seromadesis: a novel technique for the treatment of chronic seromas following breast surgery. Breast J. 2006, 12(5): 502–504.
21. Metcalfe D., Sinha S., Sadek N., et al. Successful use of talc sclerodesis to control a persistent high-output groin seroma following endovascular abdominal aortic aneurysm repair. Ann Vasc Surg. 2013, 27(6): 801.e9–801.e12.
22. Lopez-Monclus J., Artes M., Gonzalez J., et al. Failure of talc seromadesis for the treatment of subcutaneous chronic seromas after incisional hernia surgery. Scand J Surg. 2021, 110(1): 105–109.
Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článek EditorialČlánek In memoriam
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2022 Číslo 3-4- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Kombinace paracetamolu s kodeinem snižuje pooperační bolest i potřebu záchranné medikace
- Metamizol v kostce a v praxi – účinné neopioidní analgetikum pro celé věkové spektrum
- Kombinace tramadol/paracetamol zmírňuje bolest v oblasti bederní páteře a může tak zmírnit i depresi
-
Všetky články tohto čísla
- Editorial
- Evaluation of resection margins in oral squamous cell carcinoma
- 3D color doppler ultrasound for postoperative monitoring of vascularized lymph node flaps
- Preservation of supraclavicular nerve while harvesting supraclavicular lymph node flap
- Determination of the adequate vascular perfusion time of cross-leg free latissimus dorsi myocutaneous flaps in reconstruction of complex lower extremity defects
- Wichterle hydron for breast augmentation – case reports and brief review
- The ideal timing for revision surgery following an infected cranioplasty
- Adult orbital xanthogranuloma – a case report
- Mini-invasive technique of sclerotherapy with talc in chronic seroma after abdominoplasty – a case report and literature review
- Multifarious uses of the pedicled SCIP flap – a case series
- In memoriam
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Mini-invasive technique of sclerotherapy with talc in chronic seroma after abdominoplasty – a case report and literature review
- Multifarious uses of the pedicled SCIP flap – a case series
- 3D color doppler ultrasound for postoperative monitoring of vascularized lymph node flaps
- Evaluation of resection margins in oral squamous cell carcinoma
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



