-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Recurrence of breast ptosis after mastopexy – a prospective pilot study
Authors: Sisti A. 1; Dalfino G. 2; Alfieri Pica E. 3; Cuomo R. 3; Sadeghi P. 4; Nisi G. 3; Grimaldi L. 3
Authors place of work: "Santa Maria alle Scotte" Hospital, University of Siena, Italy ; Division of Plastic Surgery, University of Tennessee, Health Science Center, Memphis, TN, USA 1; Division of Otorhinolaryngology, Department of Biotechnology and Life Sciences, University of Insubria, Varese, Italy 2; Division of Plastic and Reconstructive Surgery, Department of Medicine, Surgery and Neuroscience 3; Plastic Surgery Department, Cleveland Clinic, Cleveland, OH, USA 4
Published in the journal: ACTA CHIRURGIAE PLASTICAE, 64, 1, 2022, pp. 18-22
doi: https://doi.org/10.48095/ccachp202218Introduction
Breast ptosis is the sagging of the breast and the consequent displacement of the same towards the lower part of the thorax. It is characterized by a severe volumetric deficiency of the upper pole, excess of skin in the lower pole, descent of the nipple-areola complex (NAC) and alteration of the morphology of the breast.
Age is an important risk factor probably in association with a genetic component [1]. With the advent of menopause and the consequent reduced production of estrogen and progesterone, the breast undergoes glandular hormonal regression and appears emptied and descended [1,2]. Other causal factors are smoking, weight loss, high body mass index (BMI), large bra cup size and numerous pregnancies with breastfeeding [1,3].
The various degrees of breast ptosis can be assessed through the classification of Regnault or Kirwan [2,4]. In the ex-obese patient, the breast ptosis can be classified using the Pittsburgh classification, that correlates the degree of ptosis to the recommended surgical treatment [5].
Mastopexy, also known as breast lifting, is the surgical operation aimed to reshape the ptotic breast without surgical removal of the breast parenchyma. Many mastopexy techniques have been described [6,7]; according to Di Summa et al [8], we can divide mastopexy techniques in four categories: dermal reshape mastopexy, mastopexy with glandular reshape, mastopexy with glandular reshape associated with perforator flap and mastopexy with associated supportive mesh. Recurrence of breast ptosis after mastopexy is a common event, but to the best of our knowledge no study in literature has ever measured the recurrence of breast ptosis after mastopexy. The aim of this study is to measure the recurrence of breast ptosis after mastopexy in a prospective study.
Materials and methods
Female patients affected by unilateral or bilateral moderate or severe breast ptosis (grade II and III according to classification of Regnault) were enrolled in this study. The prospective study started on 01/01/2017 and ended on 01/06/2018. A total of 10 patients were included in this study (Tab. 1).
Tab. 1. Patients’ data included in the study. 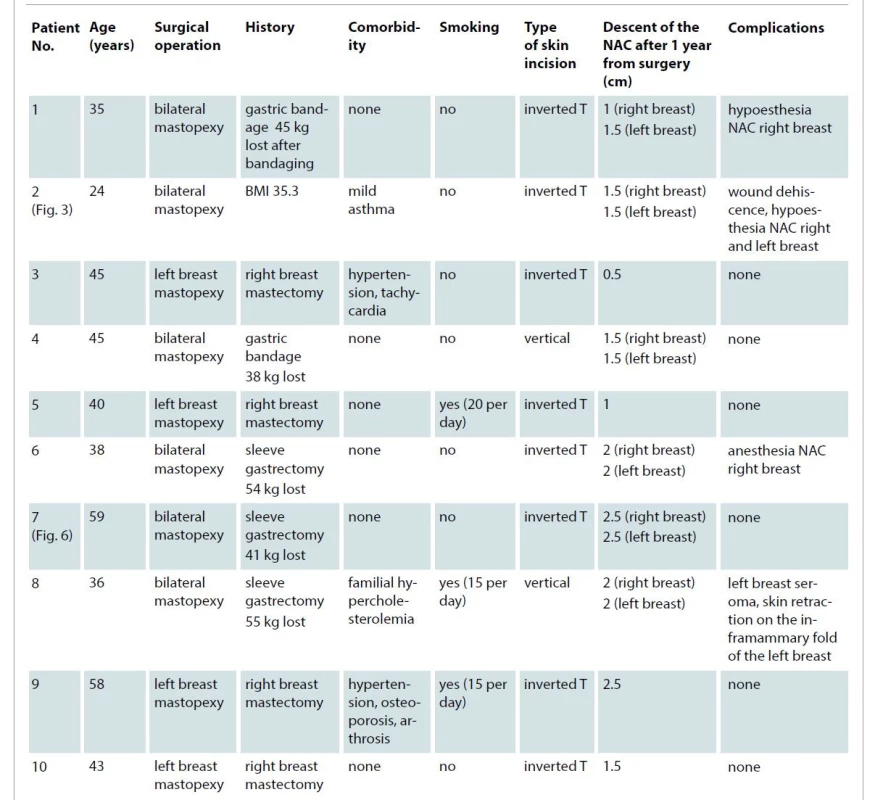
BMI – body mass index, J-C – jugular notch-nipple areola complex distance, NAC – nipple-areola complex All surgical operations were performed by the same surgeon under general anesthesia. Inverted T (Wise pattern) mastopexy was performed in all the patients: after de-epithelialization following the pre-operative drawing, the excess of skin was removed through an inverted T incision, and the NAC was lifted to the desired position without any auto-augmentation technique. At the time of the first outpatient visit, all the patients accepted the informed consent. Ethical standards were respected during the individual procedures of our Institute in accordance with the Helsinki Declaration of 1964 and his subsequent amendments. The patients were evaluated at 1 month, 3 and 6 months and 1 year after surgery. The jugular notch-nipple areola complex distance (J-C) was measured before surgery, immediately after surgery, and after 1, 2, 6 and 12 months.
Results
Ten patients were enrolled in the prospective study (Tab. 1). Four patients underwent unilateral mastopexy (for symmetrization at the same time of contralateral breast reconstruction) and 6 patients underwent bilateral mastopexy.
The J-C ranged, at the time of the pre-operative measurement, between 22 and 32 cm, with an average value of 27.25 cm (Fig. 1). This distance in the immediate post-operative period ranged between 19 and 24 cm, with an average value of 20.94 cm and a consequent average reduction of 6.31 cm (Fig. 1). The average J-C after one year was 22.6 cm and the descent of the NAC was between 0.5 and 2.5 cm, with an average of 1.69 cm ± 0.55 cm.
Fig. 1. Changes in jugular notch / nipple-areola complex distance. The measurements are expressed in centimeters. 
The lifting of the NAC, measured in the immediate post-operative period, ranged from 3 to 8.5 cm, with an average value of 6.3 cm ± 1.5 cm. This measurement, one year after surgery, ranged from 2 to 7 cm, with an average value of 4.6 cm ± 1.4 cm.
The lifting of the NAC one year after surgery compared to the immediate post-operative showed a loss between 12.5 and 41.7%, with an average value of 27.5 ± 9.4%. Fig. 2–6 represent patients pre - and post-surgery.
Fig. 2. Patient No. 1 underwent bilateral mastopexy surgery: preoperative photograph (left), immediate-postoperative (center) and one year after surgery (right). 
Fig. 3. Patient No. 2 underwent bilateral mastopexy surgery: preoperative photograph (left), immediate-postoperative (center) and one year after surgery (right). 
Fig. 4. Patient No. 4 underwent bilateral mastopexy surgery: preoperative photograph (left), immediate-postoperative (center) and one year after surgery (right). 
Fig. 5. Patient No. 5 underwent unilateral mastopexy: preoperative photograph (left), immediate-postoperative (center) and one year after surgery (right). 
Fig. 6. Patient No.7 underwent bilateral mastopexy: preoperative photograph (left), immediate-postoperative (center) and one year after surgery (right). 
Discussion
The concept of recurrence of breast ptosis is given as acquired by plastic surgeons and explained to patients before surgery as one of the possible outcomes after mastopexy. Before this study, no study in literature had ever measured the recurrence of breast ptosis after mastopexy.
Recurrence of breast ptosis is a frequent event, and we evaluated the post-operative evolution of patients’ breast, carefully examining the distance between the jugular notch and the nipple-areola complex.
Patient No. 3, 45 years old, underwent unilateral mastopexy for symmetrization during contralateral breast reconstruction, and a lifting of the NAC of 3.5 cm was reached in the immediate post-operative period. However, one year after surgery, the NAC dropped 0.5 cm, with the loss of 12.5% of the lift obtained through mastopexy. This represents the best result of our study and this was probably due to the patient's normal weight (BMI 20–25). Upon notice, patient No. 3 didn’t have bariatric surgery before the mastopexy.
Patient No. 7 (Fig. 6), 59 years old, who underwent bilateral mastopexy after bariatric surgery using the sleeve gastrectomy technique, showed a lifting of the NAC of 7 cm on the right breast and 6 cm on the left breast in the immediate post-operative time. Despite the stability of the body weight reached for some years, the patient showed a drop of the NAC of 2.5 cm in both breasts one year after surgery. The consequent loss of the lift obtained through mastopexy was 35.7% in the right breast and 41.7% in the left breast. In this case, although the patient was healthy, the recurrence of breast ptosis may have been due to the fact that the patients was a former obese.
In fact, bariatric surgery determines a significant weight loss associated with the reduction of the adipose component of the breast [1]. In these patients, other techniques with parenchymal reshape would be preferred because mastopexy with skin removal only is often inadequate to restore a pleasant shape and volume [9]. The glandular support with stitches or mesh, or the use of perforator flaps or implants, could better address the severe breast ptosis and hypoplasia associated with massive weight loss [10–19]. These other techniques can produce long-lasting results because the breast obtained does not rely only on skin envelope.
Patient No. 2 (Fig. 3), 24 years old, underwent bilateral mastopexy surgery with a lifting of the NAC of 8.5 cm in both breasts. One year after surgery, although the patient had not previously undergone any surgery, she showed a drop of the NAC of 1.5 cm in both breasts, with a 17.6% reduction of the lift achieved through mastopexy. This probably occurred because the patient had a BMI of 35.3 at the time of surgery, which corresponds to a class 1 obesity.
In general, although it is impossible to completely avoid the gravitational effect exerted by breast itself, the results one year after surgery have been satisfactory for the patients included in our case series, with the average descent of the NAC equal to 1.69 cm (average reduction of 27.5% of the lifting obtained through mastopexy).
To investigate the causes of the breast ptosis recurrence goes beyond the scope of this study. We have to acknowledge that this study has some limitations: the sample is small, and the outcomes cannot be compared with other values in literature, since no other similar study has been published so far. Furthermore, the outcomes were not statistically related to variables like the BMI or the comorbidity, because of the small sample. The follow-up time is relatively short but still significant if we think that an average lifting-loss of 27.5% occurred just in the first year after surgery.
This study is the description of our experience with mastopexy on a small number of patients and aims to be a pilot study for subsequent studies on this very important topic in plastic surgery. A more extensive study with a longer follow-up is planned. This case series represents our best effort to measure, for the first time in literature, how breast ptosis recurs after mastopexy.
Conclusion
Mastopexy is a very common plastic surgery procedure and breast ptosis after mastopexy often recurs after surgery. In our case series, the lifting of the NAC one year after surgery compared to the immediate post-operative showed a loss ranging 12.5–41.7%. Although the sample of this study is small, this pilot study aims to bring the attention of the scientific community on this common phenomenon and to encourage further studies on this topic. Patients should be informed about the possible recurrence of breast ptosis after mastopexy.
Disclosure: All procedures performed in this study involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Role of authors: Dr. Andrea Sisti, MD and Dr. Payam Sadeghi, MD contributed to this study equally.
Andrea Sisti: the main author who drafted most part of the manuscript, study design and data collection/figures production.
Gianluca Dalfino: the second main contributor in writing the manuscript, helped with the data collection and graph production.
Edoardo Pica Alfieri: contributed to writing the manuscript and editing it.
Roberto Cuomo: darfting parts of the manuscript and helped by data analysis.
Payam Sadeghi: corresponding author, drafting the manuscript and edits.
Giuseppe Nisi: manuscript revisions and review of the literature.
Luca Grimaldi: supervising the study design and English editing.
Conflict of interest: None.
Funding: None.
Payam Sadeghi, MD
Cleveland Clinic Main Campus,
Crile Building
6th Floor, Department of Plastic Surgery
9500 Euclid Ave
44195, Cleveland
Ohio, USA
e-mail: Drpayamsadeghi@yahoo.com
Submitted: 8. 11. 2021
Accepted: 6. 2. 2022
Zdroje
1. Rinker B., Veneracion M., Walsh CP. Breast ptosis: causes and cure. Ann Plast Surg. 2010, 64(5): 579–584.
2. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976, 3(2): 193–203.
3. Rinker B., Veneracion M., Walsh CP. The effect of breastfeeding on breast aesthetics. Aesthet Surg J. 2008, 28(5): 534–537.
4. Kirwan L. A classification and algorithm for treatment of breast ptosis. Aesthet Surg J. 2002, 22(4): 355–363.
5. Song AY., Jean RD., Hurwitz DJ., et al. A classification of contour deformities after bariatric weight loss: the Pittsburgh Rating Scale. Plast Reconstr Surg. 2005, 116(5): 1535–1544.
6. Hidalgo DA., Spector JA. Mastopexy. Plast Reconstr Surg. 2013, 132(4): 642e–656e.
7. Wong C., Vucovich M., Rohrich R. Mastopexy and reduction mammoplasty pedicles and skin resection patterns. Plast Reconstr Surg Glob Open. 2014, 2(8): e202.
8. di Summa PG., Oranges CM., Watfa W., et al. Systematic review of outcomes and complications in nonimplant-based mastopexy surgery. J Plast Reconstr Aesthet Surg. 2019, 72(2): 243–272.
9. D'Aniello C., Cuomo R., Grimaldi L., et al. Superior pedicle mammaplasty without parenchymal incisions after massive weight loss. J Invest Surg. 2017, 30(6): 410–420.
10. Persichetti P., Tenna S., Brunetti B., et al. Anterior intercostal artery perforator flap autologous augmentation in bariatric mastopexy. Plast Reconstr Surg. 2012, 130(4): 917–925.
11. Rubin JP., Gusenoff JA., Coon D. Dermal suspension and parenchymal reshaping mastopexy after massive weight loss: statistical analysis with concomitant procedures from a prospective registry. Plast Reconstr Surg. 2009, 123(3): 782–789.
12. Thornton DJ., Fourie le R. Autologous augmentation-mastopexy after bariatric surgery: waste not want not! Aesthetic Plast Surg. 2010, 34(4): 519–524.
13. van Deventer PV., Graewe FR., Würinger E. Improving the longevity and results of mastopexy and breast reduction procedures: reconstructing an internal breast support system with biocompatible mesh to replace the supporting function of the ligamentous suspension. Aesthetic Plast Surg. 2012, 36(3): 578–589.
14. de Bruijn HP., Johannes S. Mastopexy with 3D preshaped mesh for long-term results: development of the internal bra system. Aesthetic Plast Surg. 2008, 32(5): 757–765.
15. De Fazio D., Cingozoglu CAC. Combined mastopexy and augmentation with autologous fat grafting: first results with lipopexy. Plast Reconstr Surg Glob Open. 2020, 8(2): e1957.
16. Liu Y., Ren Y., Wu M., et al. Simultaneous mastopexy via areola excision to correct mild and moderate breast ptosis. Aesthetic Plast Surg. 2021, 45(3): 948–955.
17. Raafat SS., Ezzat SZ., Khachaba YA., et al. Autologous mastopexy and autoaugmention of the breast. Plast Reconstr Surg Glob Open. 2020, 8(10): e3126.
18. Ramanadham SR., Rose Johnson A. Breast lift with and without implant: a synopsis and primer for the plastic surgeon. Plast Reconstr Surg Glob Open. 2020, 8(10): e3057.
19. Sisti A., Tassinari J., Nisi G., et al. Superior pedicle mastopexy with the three fat-glandular flap support. Plast Reconstr Surg. 2017, 139(1): 311e–312e.
Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článek Editorial
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2022 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Kombinace paracetamolu s kodeinem snižuje pooperační bolest i potřebu záchranné medikace
- Metamizol v kostce a v praxi – účinné neopioidní analgetikum pro celé věkové spektrum
- Kombinace tramadol/paracetamol zmírňuje bolest v oblasti bederní páteře a může tak zmírnit i depresi
-
Všetky články tohto čísla
- Editorial
- Efficacy of pedicled anterolateral thigh flap for reconstruction of regional defects – a record analysis
- Depression and anxiety disorders in patients with carpal tunnel syndrome after surgery – a case control study
- Recurrence of breast ptosis after mastopexy – a prospective pilot study
- Development of a questionnaire for a patient-reported outcome after nasal reconstruction
- Breast reconstruction with autologous abdomen-based free flap with prior abdominal liposuction – a case-based review
- Superficial circumflex iliac artery perforator flap on extremity defects – case series
- Emergency evacuation low-pressure suction for the management of extravasation injuries – a case report
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Superficial circumflex iliac artery perforator flap on extremity defects – case series
- Efficacy of pedicled anterolateral thigh flap for reconstruction of regional defects – a record analysis
- Recurrence of breast ptosis after mastopexy – a prospective pilot study
- Breast reconstruction with autologous abdomen-based free flap with prior abdominal liposuction – a case-based review
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



