-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Langerhans cell histiocytosis in adults
Histiocytóza z Langerhansových buněk u dospělých
Histiocytóza z Langerhansových buněk u dospělých je vzácným onemocněním, které potenciálně může postihovat všechny orgány nebo při kterém může toto multiorgánové postižení chybět. Na našem pracovišti bylo léčeno 95 pacientů s histologicky potvrzenou LCH. V době stanovení diagnózy mělo onemocnění u více než 1/ 3 pacientů multisystémový charakter. Aktivita LCH se u přibližně 1/ 4 pacientů obnovila do 6 let (medián), obzvláště v dalších jednotlivých orgánech. Pro určení stupně závažnosti choroby a stanovení orgánového postižení je potřebná rozsáhlá diagnostika. K dispozici je řada léčebných možností, jak při postižení jednoho orgánu, tak pro léčbu systémové formy onemocnění. Je smysluplné toto onemocnění řešit interdisciplinárně.
Klíčová slova:
histiocytóza z Langerhansových buněk
Authors: C. Doberauer
Authors place of work: Department of Internal Medicine, Evangelische Kliniken Gelsenkirchen, Germany, head Prof. Dr. med. Claus Doberauer
Published in the journal: Vnitř Lék 2010; 56(Supplementum 2): 22-26
Category: Histiocytóza z Langerhansových buněk a některá další vzácná hematologická onemocnění
Summary
Langerhans cell histiocytosis in adults is a rare disease with potential involvement of all organs with or without organ dysfunction. In our single institution, 95 patients with histologically confirmed LCH were treated. At time of diagnosis, more than 1/ 3 of the patients had shown multi system disease. Reactivations of LCH occurred in about 1/ 4 of the patients within a median of 6 years, especially in other individual organs. For staging and determination of organ dysfunction extensive diagnostic is necessary. There are a lot of treatment options in relation to isolated organ involvement or systemic disease. It makes sense to approach the disease in a multidisciplinary way.
Key words:
Langerhans cell histiocytosisIntroduction
In adults, Langerhans cell histiocytosis (LCH) is a rare disease with a predominantly good prognosis. But consequences of the non malignant proliferations of Langerhans cells in organs can be dysfunctions up to organ failures. Manifestations of LCH can vary from single organ involvement, usually of lungs, bones or skin, to multiple organ involvement. So, LCH is divided into a single system disease and into a multi system disease. The symptoms are related to the organs affected. Risk organs in adults are not yet defined [1]. Only a few cases of malignant courses are described [2]. Langerhans cell sarcoma can occur as well de novo as from an antecedent LCH [3].
Exact incidence and prevalence of LCH in adults are not known. There is an estimation of one to two new manifestations per million population per year [4]. An immune defect is presumed as the likely cause of the disease. Additional influences of environment, for example smoking, were widely discussed [5]. Women are more frequent affected than men. The preferred age of manifestation is in the third to fourth decade. Accumulations in families are described.
There seems to be an association between LCH and malignant tumours. In most cases, LCH occurs before or concurrently with the associated neoplasma. The histopathology of malignant neoplasms are especially malignant lymphomas or solid tumours [6].
Patients and course of disease
From October 2000 until May 2010 95 patients with histologically confirmed LCH were treated in our single institution. Characteristics of patients are shown in tab. 1. Isolated lung manifestation only occurred in patients smoking or having smoked. At time of diagnosis, more than 1/ 3 of the patients had been suffering from multi system disease.
Tab. 1. Characteristics of patients with LCH. 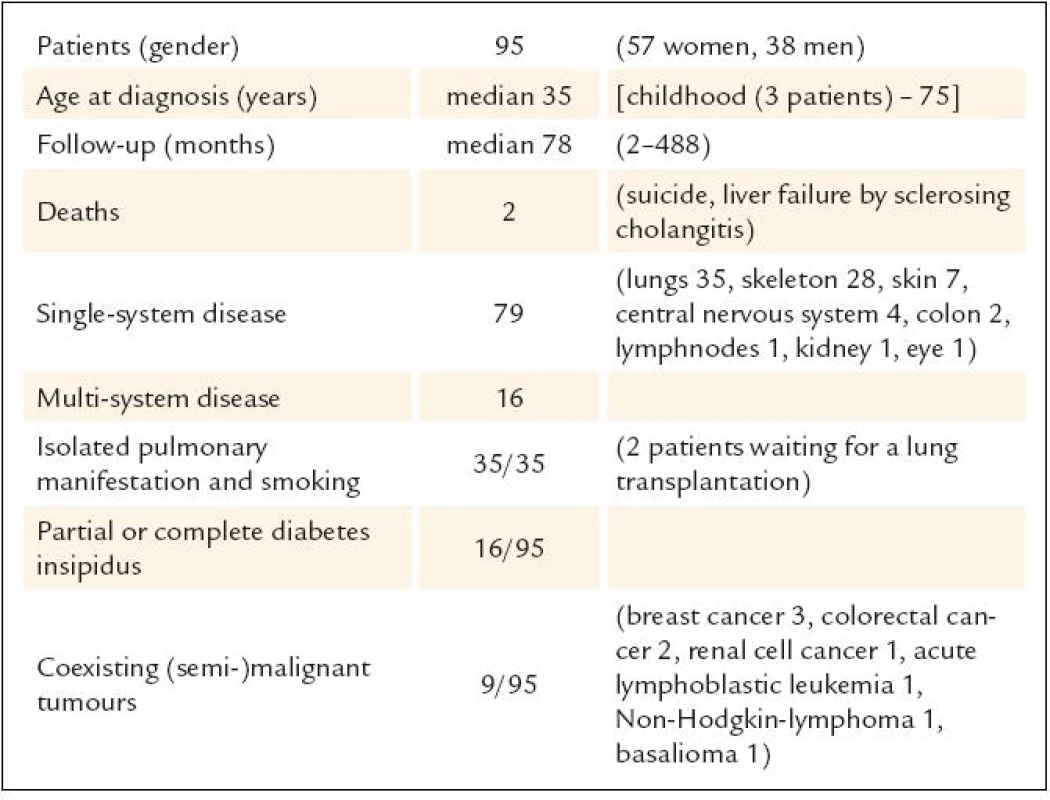
The course of LCH is variable with spontaneous remissions up to 70% in cutaneous manifestations and up to 50% in pulmonary disease. Osseous manifestations are difficult to measure. In active disease there are the categories regression, stable disease and progression. In non active disease reactivations are possible.
In 2008, we evaluated our patients with regard to reactivations (tab. 2). Reactivations of LCH in adults occurred in about 1/ 4 of the patients within a median of six years of follow up, especially in other individual organs. Eight patients have shown two to four further reactivations in course.
Tab. 2. Reactivations of LCH in adult patients. 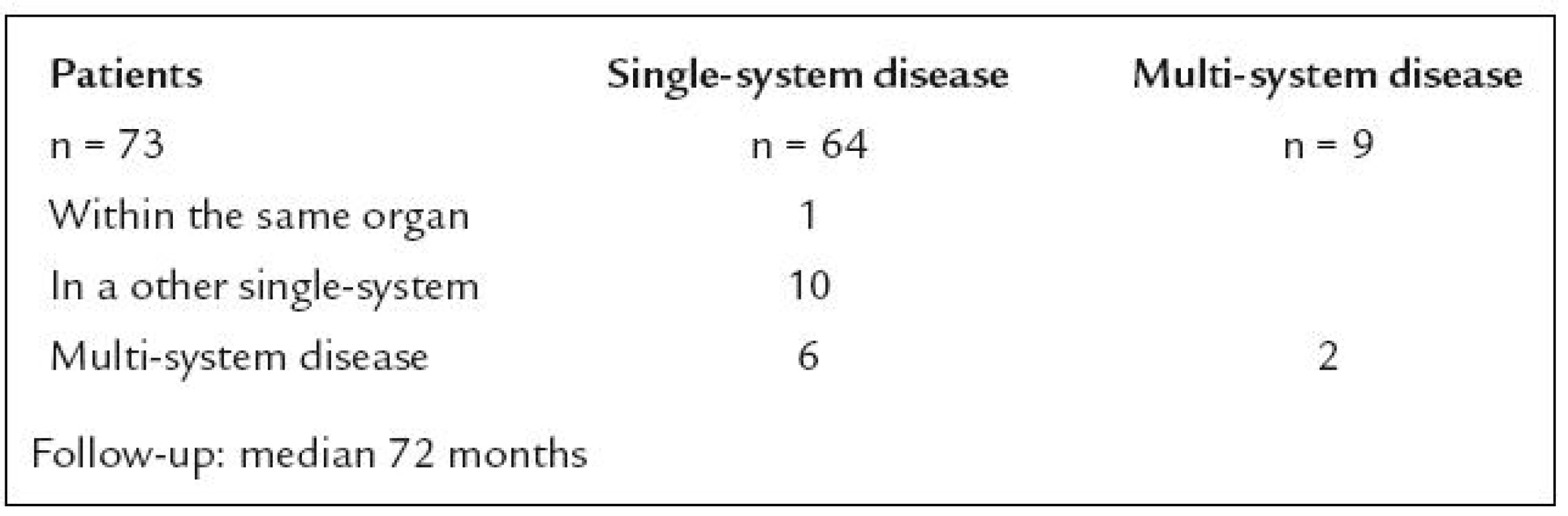
Diagnostic evaluation
For staging and determination of organ dysfunction an extensive diagnostic is necessary. The evaluation should embrace history and physical examination, especially inspection of skin and mucous membranes. Moreover, technical investigations are necessary: ultrasound of neck with thyreoid gland, abdomen and pelvis, X-ray and if need be CT scans of thorax, CT scan or NMR of skeleton, NMR of head, blood measurements and status of urine. Further investigations can be scintigraphy of bones, PET-(CT) scan, bone marrow biopsy and other investigations because of specials symptoms, for example measurements of hormones. An experimental approach is the measurements of cytokines to correlate with the activity of the disease. Typical manifestations of LCH are shown in fig. 1 – 5.
Fig. 1a, 1b. Cutaneous manifestations of LCH: disseminated brown papules on regions of increased sweating. 
Fig. 2a, 2b. Pulmonary manifestations of LCH: computerized tomography of the chest with multiple nodular foci and cystic changes of the lungs. 
Fig. 3a, 3b. Osseous manifestation of LCH: nuclear magnetic resonance tomography of the head with an eosinophilic granuloma of the skull. 
Fig. 4a, 4b. Gastrointestinal manifestations of LCH: granulomatous lesions of the mucous membrane of the stomach and the esophagus in an endoscopic view. 
Fig. 5a, 5b. Manifestations of LCH in central nervous system: magnetic resonance tomography of the head with metastases-like lesions in cerebrum. 
Treatment options and discussion
An optimal therapy for LCH in adults has not been established. But there are a lot of treatment options in relation to isolated organ involvement or systemic disease with or without organ dysfunction (tab. 3). Up to now, no controlled therapeutic studies have been performed in adults. So, approaches of therapy are following the experiences in children or take experimental results into consideration. Factors with unfavorable prognosis are advanced age, extensive organ involvement, number of organs affected, organ dysfunction and poor response to therapy. In cases of organ dysfunctions, supportive therapy is crucial.
Tab. 3. Treatment options in adults. 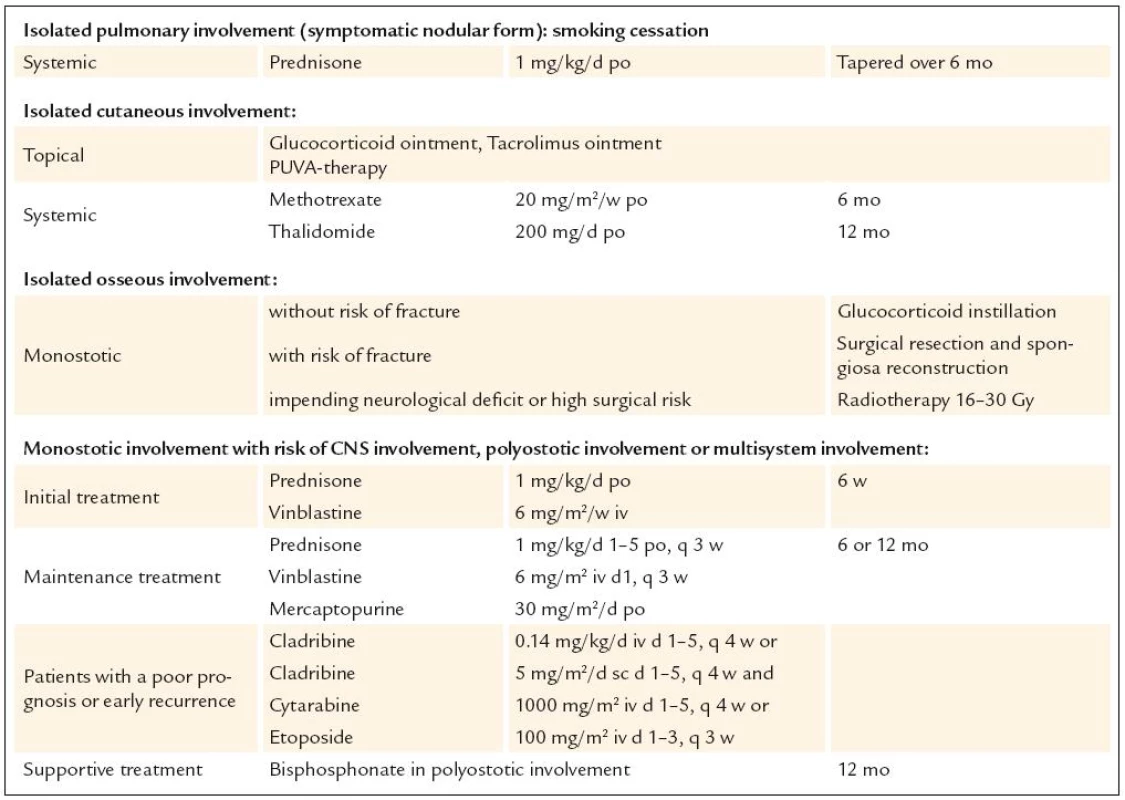
Further options of therapy seemed to be an immunomodulatoric therapy with cyclosporine or interferon, the use of monoclonal antibodies like CD1a - or CD52 - antibodies, and treatment with TNF-α-inhibitors like etanercept or infliximab. The results of these approaches were disappointing or of questionable success. In a few patients with chronic active course of LCH, an anti-inflammatoric and angiostatic therapy with rofecoxib, pioglitazone and trofosfamide resulted in long-lasting non-active disease [7]. Autologous or allogenic stem cell transplantation can lead to healing of the disease, but is fraught with high morbidity and mortality [8]. Advanced organ failure can only be treated with transplantation, for example of liver or lung, but LCH may reappear in the transplanted organ [9]. A new promising approach is the treatment with an aggressive chemotherapy resulting in long-lasting regressions [10].
Because of missing studies, the treatment of Langerhans cell sarcoma has to be individual. There are a lot of open questions. For answering these questions, further studies are warranted.
Prof. Dr. med. Claus Doberauer
www.evk-ge.de
e-mail: doberauer@evk-ge.de
Doručeno do redakce: 9. 9. 2010
Zdroje
1. Fichter J, Doberauer C, Seegenschmiedt H. Langerhans cell histiocytosis in adults: An interdisciplinary challenge. Dtsch Arztebl 2007; 104: A2347 – A2353.
2. Jülg BD, Weidner S, Mayr D. Pulmonary manifestation of a Langerhans cell sarcoma: case report and review of the literature. Virchows Arch 2006; 448 : 369 – 374.
3. Lee JS, Ko GH, Kim HC et al. Langerhans cell sarcoma arising from Langerhans cell histiocytosis: a case report. J Korean Med Sci 2006; 21 : 577 – 580.
4. Stockschlaeder M, Sucker C. Adult Langerhans cell histiocytosis. Eur J Haematol 2006; 76 : 363 – 368.
5. Vassallo R, Ryu JH, Colby TV et al. Pulmonary Langerhans’ cell histiocytosis. N Engl J Med 2000; 342 : 1969 – 1978.
6. Egeler RM, Neglia JP, Puccetti DM et al. Association of Langerhans cell histiocytosis with malignant neoplams. Cancer 1993; 71 : 865 – 873.
7. Reichle A, Vogt T, Kunz ‑ Schughart L et al. Anti‑inflammatory and angiostatic therapy in chemorefractory multisystem Langerhans’cell histiocytosis of adults. Br J Haematol 2005; 128 : 730 – 732.
8. Akkari V, Donadieu J, Piguet C et al. Hematopoietic stem cell transplantation in patients with severe Langerhans cell histiocytosis and hematological dysfunction: experience of the French Langerhans Cell Study Group. Bone Marrow Transplant 2003; 31 : 1097 – 1103.
9. Habib SB, Congleton J, Carr D et al. Recurrence of recipient Langerhans’ cell histiocytosis following bilateral lung transplantation. Thorax 1998; 53 : 323 – 325.
10. Derenzini E, Fina MP, Stefoni V et al. MACOP ‑ B regimen in the treatment of adult Langerhans cell histiocytosis: experience on seven patients. Ann Oncol 2010; 21 : 1173 – 1178.
Štítky
Diabetológia Endokrinológia Interné lekárstvo
Článok vyšiel v časopiseVnitřní lékařství
Najčítanejšie tento týždeň
2010 Číslo Supplementum 2- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Rizikové období v léčbě růstovým hormonem: přechod mladých pacientů k lékařům pro dospělé
- Statinová intolerance
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Pulmonary involvement in patients with multiorgan Langerhans cell histiocytosis. Eight case studies and literature review
- PET-CT in the diagnostics and monitoring of pulmonary Langerhans cell histiocytosis
- An overview of the treatment of Langerhans cell histiocytosis in adult patients
- Cladribine as the first line treatment in multifocal or multiorgan Langerhans cell histiocytosis in adult patients
- Radiotherapy of Langerhans’ cell histiocytosis
- Hemophagocytic lymphohistiocytosis syndrome
- Erdheim-Chester disease in pictures
- Necrobiotic xanthogranuloma – a rare cutaneous complication in a patient with multiple myeloma
- CD4+56+ leukemia from dendritic cells type DC2
- Systemic mastocytosis
- Langerhans cell histiocytosis in adults
- Langerhans cell histiocytosis: a pathologist view
- Pathology of histiocytoses of non-Langerhans cell type
- Langerhans cell histiocytosis in children and adolescents
- Slovo úvodem
- Langerhans cell granulomatosis
- Head and neck manifestation of Langerhans’ cell histiocytosis
- Langerhans cell histiocytosis (LCH) in orofacial region
- An overview of the histiocytic diseases that are a subject to this Vnitřní lékařství supplement
- Langerhans cell histiocytosis – cutaneous aspects of the disease
- CNS sequelae in Langerhans cell histiocytosis and Erdheim-Chester disease. The importance of PET-CT for the diagnostics and evaluation of treatment response
- Vnitřní lékařství
- Archív čísel
- Aktuálne číslo
- Iba online
- Informácie o časopise
Najčítanejšie v tomto čísle- Hemophagocytic lymphohistiocytosis syndrome
- Erdheim-Chester disease in pictures
- Systemic mastocytosis
- Langerhans cell histiocytosis in children and adolescents
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



