-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Classification of scapular body fractures
Klasifikace zlomenin těla lopatky
Úvod:
Cílem tohoto článku je na základě 3D CT rekonstrukcí 187 zlomenin těla lopatky navrhnout klinicky orientovanou klasifikaci zlomenin těla respektující biomechanickou stavbu lopatky.Metody:
V souboru 375 zlomenin lopatky jsme identifikovali celkem 187 zlomenin těla lopatky u 187 pacientů (157 mužů, 30 žen), průměrného věku 48 roků (range; 16−100 roků). U všech zlomenin byly provedeny 3D CT rekonstrukce umožňující objektivní zhodnocení typu zlomeniny. Operováno bylo 46 pacientů, což umožnilo korelovat peroperační nález s 3D CT rekonstrukcemi. Za zlomeniny těla jsme považovali pouze ty zlomeniny, které procházely biomechanickým tělem lopatky, tj. porušovaly alespoň jeden z pilířů. Nepatřily sem proto zlomeniny horního úhlu a horního okraje těla lopatky, neboť se jednalo o okrajové zlomeniny, které ponechávají oba pilíře intaktní. Exkludovali jsme i zlomeniny krčku lopatky, které jsou definovány jako extraartikulární dvoufragmentové zlomeniny laterálního úhlu lopatky oddělující glenoid od těla lopatky. Vyřadili jsme i zlomeniny dolního úhlu lopatky. Hodnotili jsme průběh lomných linií, jejich vztah k oběma pilířům lopatky, a počet fragmentů. Jako samostatný fragment byl hodnocen pouze takový úlomek, který nesl část obvodu biomechanického těla. Tzn., že nebyly započítány interkalární fragmenty vylomené z centrální části fossa infraspinata.Výsledky:
Identifikovali jsme tři základní skupiny zlomenin těla, tj. zlomeniny postihující pouze spinální pilíř, zlomeniny postihující pouze laterální pilíř a zlomeniny obou pilířů.
Zlomeniny spinózního pilíře jsme zaznamenali 12krát. V 8 případech probíhala hlavní lomná linie vertikálně ze supraspinátní jámy centrální částí spinálního pilíře směrem do mediálního okraje infraspinátní fossy. Ve 4 případech byla baze spina scapulae vylomena z těla lopatky. Laterální pilíř zůstal ve všech případech neporušen a dislokace fragmentů byla vždy malá, takže všechny zlomeniny byly léčeny konzervativně.
Zlomeniny laterálního pilíře se vyskytly ve 143 případech. Vždy šlo o zlomeninu infraspinátní části těla lopatky tj. infraspinátní jámy, kdy hlavní lomná linie vycházela z laterálního pilíře. Tento typ zlomeniny jsme na základě počtu obvodových úlomků rozdělili na další tři subtypy, tj. dvou-fragmentové (88 zlomenin), tří-fragmentové (31 zlomenin) a kominutivní (24 zlomenin).
Zlomenina obou pilířů byla zjištěna ve 32 případech. Tato zlomenina se vyskytovala ve dvou formách. V první skupině (11 zlomenin) probíhala lomná linie spinózním pilířem v těsné blízkosti spinomediálního úhlu do horního úhlu lopatky. Ve druhé skupině (21 zlomenin) procházela hlavní lomná linie centrálním zeslabením spina scapulae. Tento kominutivní typ zlomeniny představoval nejzávažnější poranění těla lopatky. Lomná linie procházela vždy zeslabenou centrální částí spinózního pilíře. Zlomenina laterálního pilíře byla dislokována ve všech případech více než zlomenina pilíře spinózního.Závěr:
Klasifikace zlomenin těla lopatky na základě postižení pilířů těla lopatky a je logická a jednoduchá. Vyžaduje 3D CT rekonstrukce včetně subtrakce okolních kostí. Respektuje anatomickou stavbu lopatky a může sloužit i jako terapeutické vodítko při plánování operační léčby.Klíčová slova:
scapula – lopatka – zlomeniny lopatky – zlomeniny těla lopatky – klasifikace zlomenin těla lopatky
Authors: J. Bartonicek 1; D. Klika 2; M. Tucek 1
Authors place of work: Central Military Hospital, Prague ; Department of orthopaedics, 1st Faculty of medicine Charles University 1; Department of radiology, Central Military Hospital, Prague 2
Published in the journal: Rozhl. Chir., 2018, roč. 97, č. 2, s. 67-76.
Category: Původní práce
Summary
Introduction:
The aim of this study is to present, on the basis of 3D CT reconstructions of 187 of scapular body fractures, a clinically oriented classification respecting the biomechanical architecture of the scapula.Methods:
In a series of 375 scapula fractures we identified 187 body fractures in187 patients (157 men, 30 women) with the mean age of 48 years (range; 16−100 years). 3D CT reconstructions were obtainedof all fractures, to allow an objective evaluation of the fracture pattern. A total of 46 patients were operated on and their intraoperative findings were correlated with 3D CT reconstructions. Scapular body fractures were deemed to be only those fractures that passed through the biomechanical body of the scapula, i.e. involved at least one of the pillars. Excluded from the study were fractures of the superior angle and of the superior border of the scapula as they were only marginal fractures leaving both pillars intact; scapular neck fractures defined as extra-articular two-part fractures of the lateral angle separating the glenoid from the scapular body; and fractures of the inferior angle of the scapula.
Evaluation focused on the course of fracture lines, their relationship to the two pillars, and the number of fragments. A separate fragment was considered to be only such a fragment that carried part of the circumference of the biomechanical body. The intercalary fragmentsbroken off the central part of the infraspinous fossa were not included.Results:
We identified three basic groups of scapular body fractures, i.e. those involving only the spinal pillar, those involving only the lateral pillar and fractures affecting both pillars.
Our series included 12 fractures of the spinal pillar, of these in 8 cases the main fracture line passed vertically from the supraspinous fossa of the central part of the pillar toward the medial border of the infraspinous fossa; in 4 cases the scapular spine base was broken off the scapular body. In all the cases, the lateral pillar was left intact and fragments were displaced only insignificantly. Therefore all these fractures were treated non-operatively.
A total of 143 fractures involved the lateral pillar. All of them were fractures of the infraspinous portion of the scapular body, i.e. the infraspinous fossa, with the main fracture line propagating from the lateral pillar. This fracture pattern was divided on the basis of the number of circumference fragments into three subtypes, namely two-part (88), three-part (31) and comminuted (24) fractures.
Fractures of both pillars were recorded in 32 cases. This fracture had two patterns, one (11 fractures) with a fracture line running through the spinal pillar close to the spinomedial angle to the superior angle of the scapula, and the other (21 fractures) with the main fracture line passing through the weakened central part of the scapular spine. This comminuted type was the most severe injury to the scapular body. The fracture line always propagated through the weakened central part of the spinal pillar. The fracture of the lateral pillar was displaced in all cases more than that of the spinal pillar.Conclusion:
Classification of scapular body fractures based on involvement of the pillars of the scapular body is logical and simple. It always requires a 3D CT reconstruction, including subtraction of the surrounding bones. It respects the anatomical structure of the scapula and may serve also as a therapeutic guidance in preoperative planning.Key words:
scapula − scapula fractures − scapular body fractures – classification − classification of scapular body fracturesIntroduction
Body fractures account for about 50% of all scapula fractures [1]. It is therefore surprising that such little attention is paid to pathoanatomy of these fractures, especially in view of the growing number of cases treated operatively [2−10]. The current classifications distinguish only between two patterns of body fractures, the simple and comminuted ones [11−15]. These classifications have no practical relevance as they reflect neither the anatomical structure of the scapula nor its potential operative treatment. There is no exact definition of scapular body fractures and as a result, certain fractures are misinterpreted as scapular neck fractures, so called infraglenoid neck fractures [11,16,17].
The aim of this study is to suggest, on the basis of 3D CT reconstructions of 187 of scapular body fractures, a clinically oriented classification respecting the biomechanical architecture of the scapula.
Methods
Material: In a series of 375 scapula fractures, covering the period from January 2002 till December 2016, a total of 187 body fractures were identified on the basis of the criteria listed below, in 187 patients (157 men, 30 women) with the mean age of 48 years (range; 16−100 years), (Tab. 1). 3D CT reconstructions were obtained in all the fractures to allow an objective evaluation of the fracture pattern, of these in 123 cases with subtraction of all adjacent bones and anterior, posterior, lateral and medial views; where necessary the view of the supraspinous fossa was added [18]. A total of 46 patients were operated on and their intraoperative findings were correlated with 3D CT reconstructions.
Tab. 1. Basic overview of scapular body fractures 
Notes: Fx – fracture; M – Male, F – Female, y – year, R –right, L – left, Th – therapy, Non – nonoperative, Ope – operative, Cla Fx – diaphyseal clavicle fracture. Method: Our definition of scapular body fractures is based on the outcomes of our previous study of the anatomical structure of the scapula [19]. The study has shown that the scapular body is reinforced by two pillars, the spinal and the lateral ones, which transmit compression forces to the scapular body from the glenoid. The two pillars are connected by the medial border of the scapula, constituting a triangular construct reinforcing the scapular body, which we have called the biomechanical body of the scapula. There are two areas of thinner bone along the circumference of the biomechanical body, namely the spinomedial angle and the central part of the scapular spine (Fig. 1).
Fig. 1. Architecture of the scapula and the course of fracture lines a – transilluminated scapula, posterior view; b – transilluminated scapula with resection of scapular spine, posterior view; c – transilluminated scapula, posteroinferiorview; d – fracture of spinal pillar; e – fracture of lateral pillar; f – fracture of both pillars. Red arrow – spinomedial angle, yellow arrow – central weakened area, black arrow – circumflex notch (weakened area of lateral pillar), blue arrow – horizontal muscular septum. 
Scapular body fractures were deemed to be only those fractures that passed through the biomechanical body of the scapula, i.e. involved at least one of the pillars. Excluded from the study were fractures of the superior angle and of the superior border of the scapula as they were only marginal fractures leaving both pillars intact, and scapular neck fractures, a separate group defined as extra-articular two-part fractures of the lateral angle separating the glenoid from the scapular body [20]. For reasons specified in the discussion we excluded also fractures of the inferior angle of the scapula.
Evaluation: Evaluation was based on the course of fracture lines, their relationship to the two pillars, i.e. the biomechanical body of the scapula, and the number of fragments. A separate fragment was considered to be only such a fragment that carried part of the circumference of the biomechanical body. The intercalary fragments broken off the central part of the infraspinous fossa were not included, similarly as minor interfragments from the fracture line in the lateral pillar. We also recorded associated clavicular fractures, the patients´ age and gender and the method of treatment.
Each author reviewed all radiographs and CT scans independently. In case of differing classification, consensus was reached by reviewing the respective scans together.
Results
We identified three basic groups of scapular body fractures, i.e. those involving only the spinal pillar, those involving only the lateral pillar and fractures affecting both pillars (Fig. 1d, e, f), (Tab.1).
Fractures of the spinal pillar: We recorded 12 such fractures in 6 men and 6 women, with the mean age of 48 years (range, 19−65), of these 6 on the right and 6 on the left. In 8 cases the main fracture line passed vertically from the supraspinous fossa of the central part of the pillar toward the medial border of the infraspinous fossa (Fig. 2a, 3). In 4 cases the scapular spine base was broken off the scapular body (Fig. 2b, 4). In all the cases, the lateral pillar was left intact and fragments were displaced only insignificantly. Therefore all these fractures were treated non-operatively. In 2 cases there occurred clavicular shaft fractures.
Fig. 2. Types of spinal pillar fractures a – fracture line passes through the central weakened area; b – scapular spine broken off the scapular body. 
Fig. 3. Spinal pillar fracture – fracture line passes through the central weakened area a – posterior view, b–superior view, c –anterior view. 
Fig. 4. Spinal pillar fracture – scapular spine broken off the scapular body. a – posterior view; b – posteroinferior view; c – superior view; d – anterior view. 
Fractures of the lateral pillar: This fracture pattern occurred in 143 cases, 123 men and 20 women, with the mean age of 48 years (range, 16−100), of these 72 on the right and 71 on the left. A total of 37 patients were treated operatively. All cases were a fracture of the infraspinous part of the scapular body i.e. the infraspinous fossa, with the main fracture line extending from the lateral pillar (Fig. 5). Associated clavicle fractures were recorded in 36 cases. We divided this type of fracture on the basis of the number of circumference fragments into three subtypes (Tab. 2).
Fig. 5. Types of lateral pillar fracture a – two-part fracture, 1 – superior fragment, 2 – inferior fragment; b – three-part fracture, 1 – superior fragment, 2 – medial fragment, 3 – lateral fragment, * – intercalary fragment; c – comminuted fracture, 1 – superior fragment, 2 – lateral fragment, 3 – inferior fragment, 4 – medial fragment, * – intercalary fragment. 
Tab. 2. Detail overview of scapular body fractures 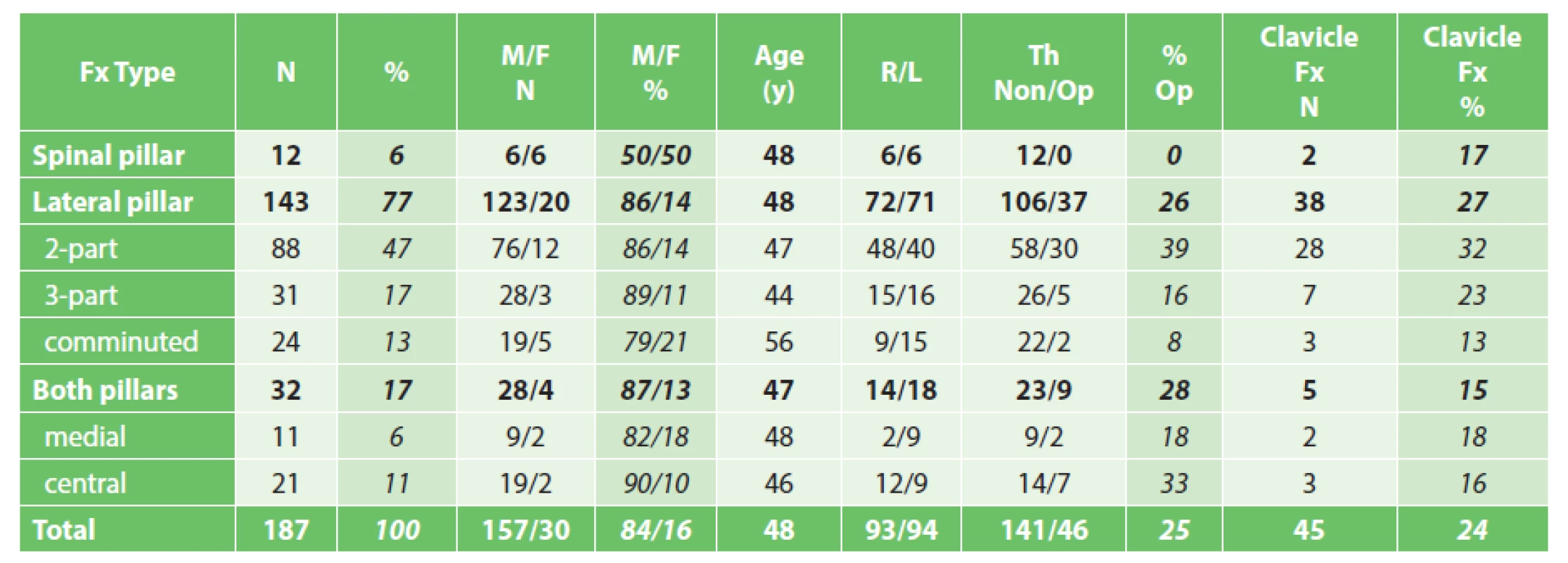
Notes: Fx – fracture, M – Male, F – Female, y – years, R –right, L – left, Th – therapy, Non – nonoperative, Op – operative, Cla Fx – diaphyseal clavicle fracture. Two-part fractures were characterized by a transversally oblique line propagating from the lateral border to the spinomedial angle. This fracture occurred in 88 cases and in 27 of them it was accompanied by a clavicle fracture. This was the most common type of scapular body fractures (47%). The course of the fracture line through the lateral pillar varied with regard to the inferior border of the glenoid. However, the fracture line always passed through the proximal half of the lateral border of the scapula, never through its distal half (Fig. 6a, b). The more distal the fracture line, the greater the tendency to angulation of the fracture and overlapping of the two main fragments of the lateral pillar (Fig. 6c, d).
Fig. 6. Types of two-part fractures of lateral pillar, different course of fracture line a – immediately below to inferior glenoid rim; b – at the level of origin of triceps long head tendon; c – through circumflex notch; d – on the border between superior and inferior half of lateral pillar. White arrow – circumflex notch, red arrow – spike of superior fragment. Notice of different types of fragment displacement (translation versus angulation with fragment overlap). 
Three-part fractures were less frequent, occurring in 31 cases; of these in 7 cases they were associated with a clavicular shaft fractures and in 1 case with AC joint dislocation. The fracture anatomy can be well seen in Fig 7.
Fig. 7. Types of three-part fracture of lateral pillar a – large inferior angle fragment, 1− glenoid fragment, 2 – inferior angle fragment, 3 – medial border fragment; b – large inferomedial fragment, 1 – glenoid fragment, 2 – lateral border fragment, 3 – large inferomedial fragment; c – large glenoid fragment, 1 – glenoid fragment, 2 – inferior angle fragment, 3 – medial border fragment,* - intercalary fragment. 
Comminuted fractures, i.e. four - and multi-part fractures, were the least frequent pattern. We recorded them only in 24 cases, of these 3times in combination with a clavicular shaft fracture. The number of fragments correlated also with the mean age of 56 years, i.e. by 8 years more than in all other types. The fracture anatomy was almost uniform. One of the fragments was formed by a part of the lateral pillar, another fragment carried the inferior angle of the scapula, and yet another fragment was avulsed from the medial border of the infraspinous part of the scapular body (Fig. 8).
Fig. 8. Types of comminuted fracture of lateral pillar (a, b, c) 1 – glenoid fragment, 2 – lateral border fragment, 3 – inferior angle fragment, 4 – medial border fragment, * - intercalary fragment. 
Fractures of both pillars: This type of fractures occurred in 32 cases, 28 men and 4 women, with the mean age of 47 years (range, 25-71), of these 14 on the right and 18 on the left. A clavicle fracture was found in 5 cases. This fracture had two patterns, one with a fracture line running through the spinal pillar close to the spinomedial angle to the superior angle of the scapula, and the other with the main fracture line passing through the central weakened area of the scapular spine (Fig. 9).
Fig. 9. Types of fractures of both pillars a – fracture involving the medial third of the spinal pillar, b – fracture involving the central part of the spinal pillar. 
Fractures involving the medial third of the spinal pillar: This fracture pattern occurred in 11 cases, 9 men and 2 women, with the mean age of 48 years (range, 25−71), of these 2 on the right and 9 on the left. Clavicular shaft was fractured in 2 patients. Three patients were operated on. A majority of fractures in this group involved the infraspinous part of the scapular body; 5times the infraspinous part of the body was split into two parts, 5times into three parts and in 1 case the fracture was comminuted.
In all 11 cases, fractures lines propagated through the medial third of the spinal pillar to the superior angle of the scapula (Fig. 10), medial to the central weakened area that always remained intact. Fracture displacement in the region of the spinomedial and superior angles of the scapula was minimal in all cases. Internal fixation of the spinomedial angle was required only in one of the three operated on cases.
Fig. 10. Fracture involving the medial third of the spinal pillar a – posterior view, b – posterosuperior view. 
Fractures involving the central part of the spinal pillar: All our cases were high-energy injuries. This fracture pattern occurred in 21 cases, 19 men and 2 women, with the mean age of 48 years (range, 27−66), of these 12 on the right and 9 on the left. A clavicle fracture was found only in 3 cases (2 fractures of the shaft, 1 fracture of the lateral clavicle). Seven patients were operated on. All of them were treated with plate fixation of both pillars.
This comminuted type of fracture was the most severe injury to the scapular body. The fracture line always propagated through the weakened central part of the spinal pillar. The fracture of the lateral pillar was displaced in all cases more than that of the spinal pillar.
We divided this fracture pattern also according to the shape of the glenoid fragment. Most frequently, in 16 cases, a large glenoid fragment was formed by the glenoid fossa, the scapular spine and the coracoid process, in 4 cases a medium-size glenoid fragment by the glenoid fossa and the coracoid process and only once by the glenoid fossa alone (Fig. 11). The size of fragments was important in terms of their reduction and fixation. The smaller the fragment, the more difficult its reduction and fixation.
Fig. 11. Fracture of both pillars, types of glenoid fragment a – glenoid fragment carrying lateral spine/acromion and coracoid process; b – glenoid fragment carrying coracoid process; c - glenoid fragment without processes. 
Course of fracture lines: Analysis of the course of fracture lines revealed their correlation with certain areas of the biomechanical triangle. In case of a fracture of the lateral pillar, all fracture lines of two-part fractures originated in its proximal half (175 cases), usually close to the sulcus circumflexus. On the medial side, most fracture lines passed toward the spinomedial angle, the weakest area of the biomechanical triangle (147 cases). Three - and multi-part fractures involved, although not so often, also the area of the junction of the middle and distal third of the medial border (Fig. 8) with a variable reinforcement in the form of a horizontal muscular septum (Fig. 1a, b). Fracture lines extended either close above or below the septum.In fractures of the spinal pillar, the fracture line propagated either through its medial third (11 cases) or, more frequently, through the weakened central area of the scapular spine (29 cases).
Clavicle fractures: These concomitant fractures were recorded in 45 cases (24%), including 42 clavicular shaft fractures and 3 fractures of the lateral clavicle. Clavicle fractures typically occurring in combination with a two-part fracture of the lateral pillar (a transverse fracture of the infraspinous fossa) were found in 28 of 88 cases (32%), and this pattern, i.e. a transverse two-part fracture associated with a clavicle fracture, accounted for 15% of all scapular body fractures.
Discussion
The first to categorize scapular body fractures was Petit who described transverse, oblique and longitudinal fractures [21]. The current schemes, including the OTA classification, distinguish only between simple (two-part) and comminuted fractures of the body [11−15, 22]. All these classifications use schematic drawings of fracture lines on the anterior surface of the scapula, without taking into account the relationship between the fracture and the anatomical structure of the scapula, i.e. the two pillars.
Older classifications, such as Ada and Miller [11], Euler and Rüedi [12,13] or OTA classification [14,15] were based merely on plain radiographs and only a minimum of patients were operated on. Only Ada and Miller [11] mentioned basic characteristics of their cohort, i.e. 148 scapula fractures in 113 patients with the mean age of 26 years (range, 5-75), 90 men and 23 women. Other studies did not specify these basic facts [12−15,22].
A recent AO study by Audigé et al. [22] was based on a series of 120 scapular body fractures, including those involving the glenoid fossa documented by 3D CT reconstructions. These reconstructions, however, were not standardized, they were obtained without subtraction of the surrounding bones and the course of fracture lines was related to the anterior surface of the scapula. It is not clear how the whole series was established and what was the time interval. The main efforts of the authors focused on analysis of the consensus of individual observers in assessment of the respective cases. The classification of scapular body fractures developed by them and fracture lines drawn on the anterior surface of the scapula do not, in our view, correspond to the reality, let alone the practical needs, as the scheme does not respect the biomechanical architecture of the scapula.
Similar deficiencies can be seen in the study by Schäfer [23], of an anonymized cohort covering the period of 2005−2010, including 115 patients with scapula fractures, with 3D CT reconstruction obtained in 91 of them.
An exceptional study was published by Armitage et al. [24], which mapped distribution of fracture lines in 90 scapula fractures documented by 3D CT reconstructions. The course of fracture lines was drawn on the posterior surface of the scapula and corresponded to the distribution of fracture lines along the circumference of the biomechanical triangle observed by us. The most frequently involved areas were those of the upper half of the lateral border of the scapula and the spinomedial angle.
The upper half of the lateral pillar is a critical site which is crossed by almost all fracture lines in case of scapular body as well as neck fractures. It is most probably the point of concentration of a direct (impact) and bending (pull of muscles) violence during the injury mechanism. It is given by the bone anatomy of the scapula, the course of muscles of the scapula (the subscapularis, the infraspinatus, the teres major) as well as by subcutaneous location of the lateral pillar which is not protected by muscles during the impact.
Our classification is based on 3D (VRT) CT reconstruction of 187 scapular body fractures concentrated by one traumacentre. It is the largest of the studies published so far. The obtained 3D CT reconstructions allowed us to assess the course of fracture lines both on the anterior and posterior surfaces of the scapula and to rule out involvement of the glenoid fossa. Our study does not include fractures of the superior angle and the superior border of the scapula which we consider as marginal fractures; fractures of the central part of the infraspinous fossa (a stab or a sharp force injury); and fissures or incomplete fractures as they are clinically irrelevant. Fractures of the lower angle were also excluded. We recorded 20 such fractures and they always involved only the distal third of the lateral border of the scapular body. Their anatomy varied, it was quite different from the above mentioned types of body fractures and will be described in a separate study. Scapular neck fractures were excluded, as well.
Unlike other classifications developed so far, showing schematic or hypothetic fracture patterns, our method produced images of real types of scapular body fractures. At the same time we respected the anatomical architecture of the scapula, its pillars in particular. Classification of fractures in view of involvement of pillars is simple and logical. It takes into account also surgical requirements, i.e. the technique of internal fixation, as the two pillars are an ideal site for fixation of implants (plates) within irregularly distributed bone mass of the scapula (Fig. 1) [6,9,19].
The most common fracture pattern in our series was a two-part fracture of the lateral pillar (fractures of the infraspinous fossa). Interpretation of this fracture in the literature is controversial as some authors term it “infraglenoid neck fracture” [7,11,16,17]. This term was introduced by Ada and Miller without any further specification [11]. Later it was used by Goss [16]. The authors were probably influenced by the fact that the fracture line extends through the lateral border of the scapula close below the glenoid (Fig. 6a, b). However, the term “infraglenoid neck fracture” is wrong. The fracture line does not separate the glenoid fossa from the scapular body, but it splits the infraspinous part of the scapular body into two parts. In addition, the fracture line never passes so close to the scapular spine base, as shown by the Goss´ drawing [16]. Another problem of this fracture pattern is the fact that it is often misinterpreted as a fracture of the surgical neck of the scapula on radiographs. And as it occurs quite frequently in combination with a clavicle fracture, it is also often confused with a floating shoulder, which ultimately leads to a number of misunderstandings [25].
In our series of fractures of both pillars, the fractures of the lateral pillar were always more displaced than those of the spinal pillar. This is given by muscle attachments. The scapular spine serves as a site for attachment of the trapezius and the deltoid muscles. These attachments reinforce the scapular spine, and the direction of pull of muscle fibres does not worsen the fracture displacement. In fractures of the lateral pillar, particularly the two-part ones, fibres of the infraspinatus, the subscapularis and the teres minor pass almost perpendicular to the fracture line of the lateral pillar. As a result their contracture leads to compression of the main fragments.
In our series of 187 fractures, a total of 47 patients (25%) were operated on. An indication for operation was a 30−40 degree angulation of the main fragments, their 100% translation, the mediolateral translation of more than 1cm and glenopolar angle (GPA) less than 20 degree, taking into account the patient´s age and general and local conditions [6, 8]. The most frequently operated on fracture pattern were two-part fractures of the lateral pillar (36%) and fractures of both pillars (33%). Fractures of the spinal pillar included in our series were not operated on due to a minimal displacement. However, these facts are somewhat approximate, as not all fractures that would require operation were operated on, either for general (polytrauma, age) or exceptionally for local reasons.
Fractures of the lateral pillar always required reduction and fixation of fragments of the lateral border of the scapular body. In fractures of both pillars with involvement of the central part of the spinal pillar, it was always necessary to use internal fixation of both pillars. An important factor in this context was the shape of the glenoid fragment. The smaller it was, the more difficult was its reduction and fixation. A more detailed analysis of the operative treatment, however, goes beyond the scope of this study.
Conclusion
Classification of scapular body fractures based on involvement of the pillars of the scapular body is logical and simple. It always requires a 3D CT reconstruction, including subtraction of the surrounding bones. It respects the anatomical structure of the scapula and may serve also as a therapeutic guidance in preoperative planning.
Conflict of interests
The authors declare no conflict of interest in connection with this article; the authors also declare that this paper has not been published in any other journal.
prof. MUDr. Jan Bartoníček, DrSc.
Department of orthopaedics,
1st Faculty of medicine Charles University,
Central Military Hospital
U Vojenské nemocnice 1200
169 02 Prague 6
Czech Republic
e-mail: bartonicek.jan@seznam.cz
Zdroje
1. Tuček M, Bartoníček J, Klika D, et al. Epidemiology of scapular fractures. ActaOrthop Belg. 2017;83 : 8−15.
2. Hardegger F, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg [Br] 1984;66-B:725−31.
3. Hersovici D, Roberts CS. Scapula fractures: to fix or not to fix? J Orthop Trauma 2006;20 : 227−9.
4. Lantry JM, Roberts CS, Giannoudis PV. Operative treatment of scapular fractures: A systematic review. Injury 2008;39 : 271−83.
5. Zlowodski M, Bhandari M, Zelle BA, et al. Treatment of scapula fractures: systematic review of 520 fractures in 22 case series. J Orthop Trauma 2006;20 : 230−3.
6. Bartoníček J, Frič V. Scapular body fractures: Results of the operative treatment. Inter Orthop 2011;35 : 747−53.
7. Cole PA, Gauger EM, Herrera DA, et al. Radiographic follow-up of 84 operatively treated scapula neck and body fractures. Injury 2012;43 : 327−33.
8. Cole PA, Gauger EM, Schroder LK. Management of scapular fractures. J Am Acad Orthop Surg 2012;20 : 130−41.
9. Bartoníček J, Tuček M, Naňka O. [Scapular fractures.] Rozhl Chir 2015;94 : 393−404.
10. Schroder LK, Gauger EM, Gilbertson JA, et al. Functional outcomes after operative management of extra-articular glenoid neck and scapular body fractures. J Bone Joint Surg Am 2016;98 : 1623−30.
11. Ada JR, Miller ME. Scapula fractures. Analysis of 113 cases. Clin Orthop Rel Res 1991;269 : 174−80.
12. Euler E, Habermeyer P, Kohler W, et al. Skapulafrakturen - Klassifikation und Differentialtherapie. Orthopäde 1992;21 : 158−62.
13. Euler E, Rüedi T. Skapulafraktur. In Habermeyer P, Schweiberer L (eds). Schulterchirurgie. München, Urban und Schwarzenberg 1996.
14. Orthopaedic Trauma Association. Fracture and dislocation compendium. Scapula fractures. J Orthop Trauma 1996; Suppl 1: S81−S84.
15. Orthopaedic Trauma Association. Fracture and dislocation compendium. Scapular fractures. J Orthop Trauma 2007;Suppl 1: S68−S71.
16. Goss TP. Fractures of glenoid neck. J Shoulder Elbow Surg 1994;3 : 42–52.
17. Goss TP. Scapula fractures and dislocations: Diagnosis and treatment. J Am Acad Orthop Surg 1995;3 : 22−33.
18. Chochola A, Tuček M, Bartoníček J, et al. [CT-diagnostic of scapular fractures]. Rozhl Chir 2013;92 : 385−8.
19. Tuček M, Bartoníček J, Frič V. [Osseous anatomy of scapula: Its importance for classification of scapular body]. Ortopedie 2011;5 : 104−9.
20. Bartoníček J, Tuček M, Frič V, et al. Fractures of the scapular neck. Diagnosis - -Classifications-Treatment. Inter Orthop 2014;38 : 2163−73.
21. Bartoníček J, Cronier P. History of the treatment of scapular fractures. Arch Orthop Trauma Surg 2010;130 : 83−92.
22. Audigé L, Kellam JF, Lambert S, et al. The AO Foundation and Orthopaedic Trauma Association (AO/OTA) scapula fracture classification system focus on body involvement. J Shoulder Elbow Surg 2014;23 : 189−96.
23. Schäfer D. Diagnostik und Klassifikation der Skapulafraktur Bedeutung der 3D-CT-Rekonstruktionen unter Anwendung der neuen AO/OTA-Klassifikation. Inaugural-Dissertation. Hohe Medizinische Fakultät der Universitätzu Köln. Köln 2015.
24. Armitage BM, Wijdicks CA, Tarkin IS, et al. Mapping of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am 2009;91 : 2222−8.
25. DeFranco MJ, Patterson BM. The floating shoulder. J Am Acad Orthop Surg 2006;14 : 499−509.
Štítky
Chirurgia všeobecná Ortopédia Urgentná medicína
Článok vyšiel v časopiseRozhledy v chirurgii
Najčítanejšie tento týždeň
2018 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
-
Všetky články tohto čísla
- Poranění pohybového aparátu
- Classification of posterior malleolar fractures in ankle fractures
- Fractures of the fifth metatarsal base
- Classification of scapular body fractures
- Anatomy of fractures of the inferior scapular angle
- Quality of nephrolithiasis surgical treatment – what is it influenced by?
- Our experience with left-sided retroperitoneal approach to resection of abdominal aortic aneurysm
- The effect of circulating tumor cells on the survival of patients with pancreatic cancer − 5-year results
- Rozhledy v chirurgii
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Fractures of the fifth metatarsal base
- Classification of posterior malleolar fractures in ankle fractures
- Classification of scapular body fractures
- Anatomy of fractures of the inferior scapular angle
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



