-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Pitva případu protrženého aneuryzma slezinné tepny
An Autopsy case of Rupture of an Aneurysm of the Splenic Artery
We present here a case of sudden death resulting from the rupture of an aneurysm of the splenic artery. From the histopathological findings, we concluded that the formation of the splenic aneurysm was associated with the fibromuscular dysplasia.
Keywords:
aneurysm – fibromuscular dysplasia – splenic artery – sudden death
Autori: Hiroshi Kinoshita; Akira Kubota; Shogo Kasuda; Minori Nishiguchi; Motonori Takahashi; Harumi Ouchi; Takako Minami; Nao Otsu; Shie Yoshida; Nobuyuki Adachi; Kiyoshi Matsui; Takehiko Yamamura; Hiroyuki Motomura; Shigeru Hishida
Pôsobisko autorov: Department of Legal Medicine, Hyogo College of Medicine, 1-1 Mukogawa-cho, Nishinomiya, Hyogo, 663-8501, Japan
Vyšlo v časopise: Soud Lék., 53, 2008, No. 4, p. 44-45
Súhrn
Prezentujeme případ náhlé smrti, jejíž příčinou bylo protržné aneuryzma slezinné tepny. Z histopathologického vyšetření vyplývá, že vznik slezinného aneuryzmatu souvisí s fibromuskularní dysplazii.
Key words:
aneuryzma – fibromuscularní dysplazie – slezinná tepna – náhlá smrtIntroduction
A splenic artery aneurysm (SAA) is a one of the most common aneurysms in the visceral artery, although its incidence is still rare (10). Here we report a case of sudden death due to a rupture of a splenic artery aneurysm.
Case Report
A 32 year old male with no remarkable past medical history was found dead in his room. An autopsy was performed to clarify the cause of death.
The deceased was a slender Japanese male, 176 cm in height and 56 kg in weight. At autopsy, no external injury was observed. The abdominal cavity was filled with approximately 2000 ml of blood with coagula. There was an aneurysm in a distal portion of the splenic artery, approximately 4cm in diameter, the lower portion of which was ruptured (Figure 1). The heart, weighing 275g contained 30ml of blood without coagula and the brain weighed 1350g, neither having any abnormal findings. No morphological abnormality of the liver (organ weight 1230g), or spleen (organ weight 125g) was observed. No aneurysm was observed in the other arteries. There were no notable changes in the other organs.
Obr. 1. Gross appearance of the splenic artery aneurysm (arrow) 
The rupture site of the aneurysm showed bleeding to the surrounding tissues (Figure 2 (a)). The normal structure of the arterial wall was destroyed with a withdrawal of the internal elastic lamina (Figure 2 (b)). Hyperplasia of the intima, muscular hypertrophy and fibrosis of media were observed. No lesions such as atheromatous plaque, calcification, periarterial inflammation, fibrinoid necrosis, mucoid medial degeneration, dissection and vacuolar degeneration of the medial smooth muscle cells were observed. Histopathological findings of the aneurysm revealed fibromuscular hyperplasia, corresponding to medial fibromuscular dysplasia. No inflammatory changes were present. No fibrosis or inflammatory change was observed in the liver, and there were no inflammatory changes or calcification in the pancreas.
Obr. 2. Cross section of the splenic artery aneurysm (a; H&E staining) and destruction of the internal elastic lamina (b; EVG staining, objective x2) 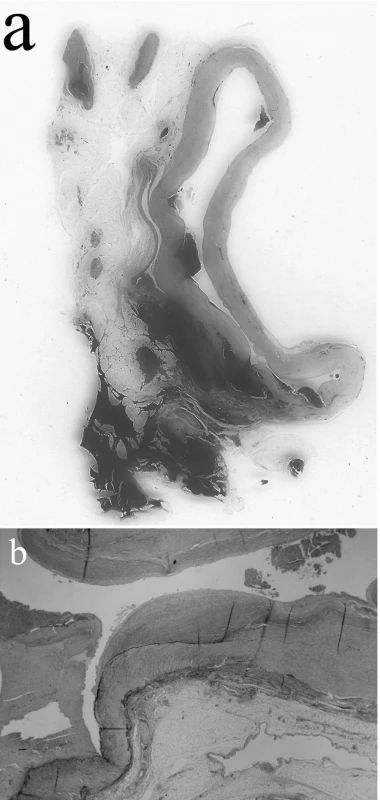
Toxicological Analysis:Toxicological screening using a TriageTMDrugs of Abuse panel plus Tricyclic Antidepressants (Biosite Diagnostic Inc., San Diego) was negative. No ethanol was detected from the blood.
Results and Discussion
SAA is the third most common intra-abdominal aneurysms, following aneurysms of the infrarenal aorta and iliac arteries (8, 11). The incidence of SAA varies from 0.01-0.2% in autopsy studies (1, 7, 8, 10, 11), to 0.78% in a study of angiography (9). Most SAA are solitary, and approximately 80% are located in the distal portion of the splenic artery (10,11). It is usually asymptomatic, and found incidentally (3, 10). Spontaneous rupture is one of the complications of SAA. Although the true incidence of rupture is difficult to ascertain, it is said to be from 3–10% in some studies, to 28% for giant aneurysm (2, 5, 9, 10).
Although the pathogenesis of SAA is poorly understand, it has been reported that various contributing factors are associated with SAA formation, including arterial fibrodysplasia, portal hypertension with splenomegaly, arteriosclerosis, inflammatory process, multiple pregnancies, blunt trauma, connective tissue disease and mycotic aneurysm (3, 6, 8–11). In the present case, portal hypertension, arteriosclerosis and pancreatitis were excluded, based on macroscopic and histopathological findings of the liver, pancreas, spleen and splenic artery. Histological changes involving arteriosclerosis are observed in up to 99% of SAA, but are most likely secondary events (5, 9). Traumatic SAA was also excluded, since the victim had no history of trauma and there were no external injuries.
Histological SAA findings revealed fibromuscular dysplasia, which is associated with the formation of SAA (12). Fibromuscular dysplasia is a non-arteriosclerotic, non-inflammatory vascular disease, involving medium or small arteries such as the renal, carotid and vertebral arteries (4). Fibromuscular lesion of the splenic artery is relatively rare (4). It is characterized by focal abnormalities in the structure of the arterial wall, and classified by the dominant site of dysplasia in the arterial wall. Although, the pathogenesis of fibromuscular dysplasia is not well understood, humoral, mechanical and genetic factors as well as mural ischemia may play a role (4).
From the macroscopic and histological findings, we concluded that the cause of death was hemorrhage in the abdominal cavity due to rupture of the SAA, associated with fibromuscular dysplasia.
All correspondence concerning this paper should be addressed to:
Dr. H. Kinoshita,
Department of Legal Medicine, Hyogo College of Medicine,
1-1, Mukogawa-cho, Nishinomiya, Hyogo, 663-8501, Japan
TEL: +81-798-45-6578, FAX: +81-798-49-3279
e-mail: kinochin@hyo-med.ac.jp
Zdroje
1. Babb RR.: Aneurysm of the splenic artery. Arch Surg 1976; 111 : 924-925.
2. Bornet P, Medjoubi S-A, Tissot A, Jurado A, Hibson J, Terris C.: Giant aneurysm of the splenic artery a case report. Angiology 2000; 51 : 343-347.
3. de Vries JE, Schattenkerk ME, Malt RA.: Complications of splenic artery anerysm other than intraperitoneal rupture. Surgery 1982; 91 : 200-204.
4. Lüscher T, Lie JT, Stanson AW, Wayne Houser O, Hollier LH, Sheps SG.: Arterial fibromuscular dysplasia. Mayo Clin Proc 1987; 62 : 931-952.
5. Matter SG, Lumsden AB.: The management of splenic artery aneurysms: experience with 23 cases. Am J Surg 1995; 169 : 580-584.
6. Safioleas M, Misiakos EP, Kakisis J, Manti C, Tsinari KK, Bakonyi Neto A.: Splenic artery aneyrysm rupture. Acta Chir Belg 1999; 99 : 306-308.
7. Saw EC, Arbegast NR, Schmalhorst WR, Comer TP.: Splenic artery aneurysms. Arch Surg 1973; 106 : 660-662.
8. Spittel JA Jr, Fairbairn JF @, Kincard OW, ReMine WH.: Aneurysm of the splenic artery. JAMA 1961; 175 : 452-456.
9. Stanley JC, Fry WJ.: Pathogenesis and clinical significance of splenic artery aneurysms. Surgery 1974; 76 : 898-909.
10. Trastek VF, Pairolero PC, Joyce JW, Hollier LH, Bernatz PE.: Splenic artery aneurysms. Surgery 1982; 91 : 694-699.
11. Trastek VF, Pairolero PC, Bernatz PE.: Splenic artery aneurysms. World J Surg 1985; 9 : 378-383.
12. Tsokos M, Nolting R-O, Lockemann U.: Sudden unexpected death due to splenic artery aneurysm rupture. Am J Forensic Med Pathol 2005; 26 : 83-95.
Štítky
Patológia Súdne lekárstvo Toxikológia
Článok vyšiel v časopiseSoudní lékařství

2008 Číslo 4
Najčítanejšie v tomto čísle- Tafonomické aspekty kadaveróznych zmien u mŕtvol uložených do zeme v plastových obaloch
- Pitva případu protrženého aneuryzma slezinné tepny
- Posudky tělesného poranění při vyšetřování trestného činu
- Recenze
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



